When someone starts forgetting where they put their keys-or worse, forgets your name-it’s easy to brush it off as just aging. But when those lapses turn into repeating the same question 20 times in an hour, getting lost in your own neighborhood, or no longer recognizing your children, it’s not normal forgetfulness. It’s Alzheimer’s disease. And it doesn’t just steal memories-it reshapes lives, for the person living with it and everyone around them.
What Happens in the Brain When Alzheimer’s Takes Hold
Alzheimer’s isn’t just about forgetting names. It’s a slow, silent war inside the brain. Two abnormal proteins start building up: amyloid-beta forms sticky plaques between nerve cells, and tau twists into tangled fibers inside them. These clumps choke off communication between brain cells, especially in the hippocampus-the area responsible for making new memories. Over time, entire regions of the brain shrink. By the time symptoms show up, damage has already been going on for 10 to 20 years.That’s why early detection matters. Blood tests are now being developed that can spot these proteins before memory problems appear. In 2023, the FDA approved lecanemab, the first drug proven to slow cognitive decline by clearing amyloid plaques. It’s not a cure, but it’s a step toward stopping the disease before it destroys too much. Still, most people won’t get this treatment. It costs thousands, requires monthly infusions, and carries risks like brain swelling. For now, the main tools doctors use are donepezil and memantine-medications that help with symptoms but don’t change the course of the disease.
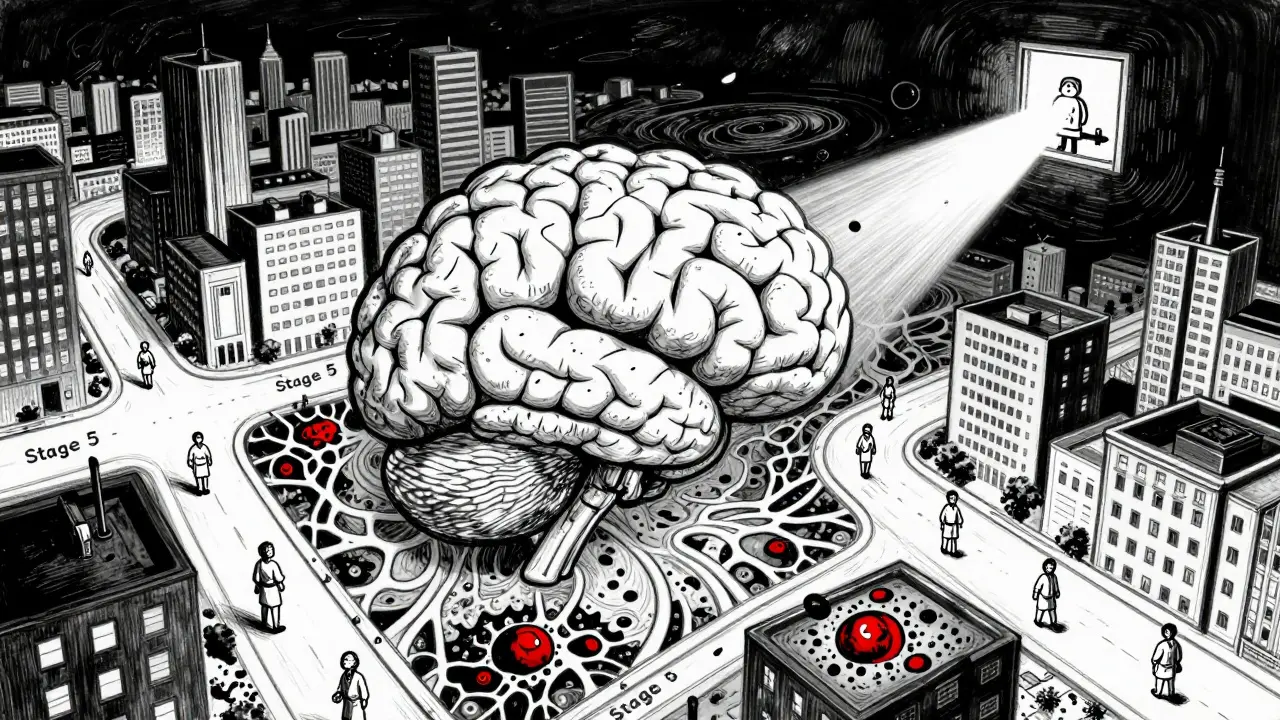
The Five Stages of Memory Decline
Alzheimer’s doesn’t hit all at once. It creeps in, then builds. Experts break it down into five stages, though not everyone follows them exactly. Progression varies-some decline fast, others hang on for years.Stage 1: Preclinical - No symptoms yet. But brain scans or blood tests may show plaques and tangles. This is the window where future treatments might work best-if we can identify it early enough.
Stage 2: Mild Cognitive Impairment (MCI) - This is where families start noticing things. A person forgets recent conversations, misplaces items constantly, or struggles to find the right word. They might repeat questions or get lost driving to a familiar store. They still remember their childhood, recognize loved ones, and can manage bills or cook meals. But they’re aware something’s wrong. That awareness brings anxiety, frustration, even denial.
Stage 3: Mild Dementia - Memory loss becomes more obvious. They forget birthdays, appointments, even their own address. They can’t plan meals or follow a recipe. They may accuse family members of stealing their things. Sleep flips-awake all night, napping during the day. Wandering becomes a risk. This stage can last years. It’s often the hardest for caregivers because the person is still alert enough to be confused, angry, or scared by their own mistakes.
Stage 4: Moderate Dementia - Now, they need help with everything: picking out clothes, bathing, using the toilet. Language breaks down. They say “the thing for hair” instead of comb. They forget how to swallow properly. Incontinence sets in. Hallucinations or delusions appear-seeing strangers in the mirror, believing they’re back in their old home. Agitation spikes. This is when many families start looking at professional care.
Stage 5: Severe Dementia - The person can’t speak. They don’t respond to names. They can’t walk without help. They’re bedbound. They lose control of muscles. Eating becomes dangerous-food gets stuck, leading to pneumonia. They may smile when touched, cry when music plays, but they can’t tell you why. This stage is physically exhausting for caregivers. But emotionally, some families say it’s quieter. The person isn’t fighting anymore.
How Caregivers Can Adapt at Each Stage
Caring for someone with Alzheimer’s isn’t about fixing things. It’s about adapting.In early stages: Focus on independence. Use sticky notes, phone alarms, labeled drawers. Keep routines steady-same breakfast time, same route for walks. Don’t correct every mistake. If they think they’re in 1978, let them. Arguing just causes stress. Encourage them to stay active-socializing, gardening, listening to old music. These things help preserve their sense of self.
In middle stages: Safety becomes priority one. Install door alarms. Remove throw rugs. Lock up knives and cleaning supplies. Use simple, one-step instructions: “Let’s wash your hands,” not “Can you go to the bathroom and wash your hands with soap?” Avoid overwhelming them with choices. Offer two shirts, not the whole closet. Validate their feelings. If they’re scared, say, “I’m here with you,” not “There’s nothing to be afraid of.”
In late stages: Comfort is everything. Soft lighting. Gentle touch. Familiar songs. A warm blanket. Even if they can’t speak, they still feel. Hold their hand. Sing to them. Play recordings of grandchildren’s voices. Manage pain-even if they can’t say it, they might grimace or pull at their clothes. Work with hospice if needed. Medicare covers up to five days of respite care per year for families who need a break.

The Hidden Toll on Caregivers
Caregivers are often invisible. They’re the ones cleaning up after accidents, sitting up all night, skipping doctor appointments for themselves. In 2023, the average caregiver spent 27 hours a week helping a loved one with Alzheimer’s. Nearly 40% said their emotional stress was high or very high. One in three reported physical strain-back pain from lifting, exhaustion from sleep loss.Many feel guilty. Guilty for getting angry. Guilty for wanting a break. Guilty for not doing enough. On online forums, caregivers share raw truths: “I yelled at her yesterday because she kept asking if her mother was dead. She died 30 years ago.” “I hid the car keys because she tried to drive to work again.” “I cried in the shower because I didn’t know how much longer I could do this.”
But there’s hope. Support groups, even virtual ones, help. Validation therapy-accepting their reality instead of correcting it-reduces conflict. Music therapy calms agitation. Even small breaks-15 minutes to sip tea alone-make a difference.
What’s Changing in Alzheimer’s Care
The old way of thinking was: “It’s just dementia. Nothing can be done.” That’s changing. Researchers are now testing drugs that target tau proteins, inflammation, and metabolism-not just amyloid. Blood tests for early detection are coming fast. Within five years, a simple finger-prick test could tell if someone is on the path to Alzheimer’s.But access is unequal. These new tests cost $3,000 to $5,000. Most people can’t afford them. Insurance doesn’t cover them yet. And in rural areas or low-income communities, specialist doctors are scarce. The disease doesn’t care about your zip code-but the care system does.
One thing is clear: Alzheimer’s isn’t just a medical issue. It’s a social one. It needs better funding for home care, paid family leave, and community support programs. It needs more training for nurses, aides, and even police officers who respond to wandering calls.
What You Can Do Today
If you’re caring for someone with Alzheimer’s, you’re not alone. Reach out. Call the Alzheimer’s Association helpline. Join a local support group. Ask for help-even if it’s just someone to sit with your loved one for an hour so you can nap.If you’re worried about memory changes in yourself or a family member, don’t wait. See a doctor. Get tested. Early diagnosis means more time to plan, more access to support, and a better shot at new treatments.
And if you’re lucky enough to still have your memories-cherish them. Call your parents. Write down stories. Say “I love you” out loud. Because one day, those moments might be all that’s left.
Is Alzheimer’s the same as dementia?
No. Dementia is an umbrella term for memory loss and cognitive decline caused by different diseases. Alzheimer’s is the most common type, making up 60-80% of cases. Other types include vascular dementia, Lewy body dementia, and frontotemporal dementia. Each affects the brain differently. For example, frontotemporal dementia often starts with personality changes or language problems, not memory loss.
Can you prevent Alzheimer’s?
There’s no guaranteed way to prevent it, but certain habits lower your risk. Regular exercise, especially walking or swimming, helps. Eating a Mediterranean-style diet-full of vegetables, fish, nuts, and olive oil-supports brain health. Managing blood pressure, diabetes, and cholesterol matters too. Staying socially active and mentally engaged-reading, playing cards, learning a new skill-also helps. It’s not about doing one thing perfectly. It’s about building healthy habits over time.
How long do people live after an Alzheimer’s diagnosis?
It varies widely. On average, people live 4 to 8 years after diagnosis, but some live up to 20 years. Age at diagnosis matters. Someone diagnosed at 65 may live longer than someone diagnosed at 85. Health also plays a role. People who stay active, eat well, and avoid complications like infections or falls tend to live longer. The disease itself doesn’t kill most people-it’s the complications: pneumonia from swallowing problems, blood clots from being bedridden, or infections from untreated pressure sores.
What should I do if my loved one keeps wandering?
Wandering is common in the middle stages. Install door alarms, lock outside doors, and hide car keys. Use GPS trackers-some are built into watches or shoe inserts. Make sure they wear an ID bracelet with their name and your phone number. Let neighbors and local police know they have Alzheimer’s. If they do go out, don’t chase them-calmly call their name, speak slowly, and offer a snack or drink. Often, they’re not lost-they’re trying to get to a familiar place from their past, like their old home or workplace.
Are there any new treatments on the horizon?
Yes. Lecanemab and donanemab are the first drugs shown to slow decline by removing amyloid plaques. Donanemab is expected to be approved in 2024. Researchers are also testing drugs that target tau tangles, reduce brain inflammation, and improve energy use in brain cells. Blood tests for early detection are being rolled out in clinical trials. The biggest shift is moving from treating symptoms to stopping the disease before it causes major damage. But these treatments are expensive and not yet widely available. Access remains a major challenge.
How can I take care of myself as a caregiver?
You can’t pour from an empty cup. Schedule regular breaks-even 20 minutes a day. Use respite care services through Medicare or local nonprofits. Talk to someone-a counselor, a friend, a support group. Don’t feel guilty for feeling angry or exhausted. It’s normal. Eat well, sleep when you can, and keep up with your own doctor visits. If you’re neglecting yourself, you won’t be able to care for your loved one for long. Asking for help isn’t weakness-it’s survival.


Nupur Vimal
December 16, 2025 AT 10:05My aunt had this and we just let her watch old Bollywood films all day she’d smile at the music even when she forgot who we were
no need to correct her just be there
Benjamin Glover
December 17, 2025 AT 12:58Another American article pretending Alzheimer’s is a crisis only the West faces. India has been managing dementia at home for centuries without your expensive infusions.
RONALD Randolph
December 18, 2025 AT 18:23Let me be perfectly clear: the FDA’s approval of lecanemab is a monumental breakthrough-despite the fact that 87% of Americans still can’t access it due to insurance red tape, bureaucratic inertia, and pharmaceutical monopolies. This isn’t science-it’s a profit-driven farce.
Mike Nordby
December 20, 2025 AT 13:51It’s important to recognize that the progression of Alzheimer’s is not linear. Cognitive decline varies significantly based on genetic predisposition, vascular health, and socioeconomic factors. Early biomarker detection via blood tests offers a paradigm shift, but implementation equity remains a critical challenge.
John Samuel
December 21, 2025 AT 12:44Every time I see someone with Alzheimer’s light up at a familiar song… I cry. Not because it’s sad, but because it’s magic. 🎶
Even when the mind fades, the heart remembers. Music isn’t just therapy-it’s a lifeline. And yes, I’ve played ‘My Way’ for my grandma for three years straight. She still taps her foot.
Sai Nguyen
December 23, 2025 AT 06:53Why do Westerners always need a drug for everything? In my village, we just keep the elders close, feed them turmeric, and let them sleep in the sun. No pills. No hospitals. Just love.
Lisa Davies
December 23, 2025 AT 19:54My mom’s a caregiver and she just started using a smart speaker to play her dad’s favorite jazz. He hasn’t spoken in months-but he smiles every time ‘Take Five’ comes on. You’re not alone. And you’re doing better than you think. 💪❤️
Melissa Taylor
December 24, 2025 AT 03:37There’s so much hope in this. Even if we can’t stop Alzheimer’s yet, we can still give people dignity. A warm blanket. A hand held. A song sung. Those aren’t small things-they’re everything.
Christina Bischof
December 25, 2025 AT 07:28i just sat with my uncle for 4 hours last week. he kept asking where his wife was. i said she was at the store. he nodded. we watched birds outside. no need to fix it. just be there.
Jocelyn Lachapelle
December 26, 2025 AT 11:52My dad was diagnosed at 72. We moved him home. We painted the walls yellow. We put his old records on. He started humming again. He didn’t remember my name-but he remembered the rhythm. That’s the part they don’t tell you. The soul doesn’t forget.
Cassie Henriques
December 28, 2025 AT 11:23The amyloid hypothesis is being challenged by emerging tau-centric and neuroinflammatory models. Recent phase 3 trials (e.g., TRAILBLAZER-ALZ 3) suggest that targeting microglial activation may yield better outcomes than plaque reduction alone. Biomarker stratification is now essential for clinical trial enrollment.
Jake Sinatra
December 29, 2025 AT 16:05Respite care under Medicare is underutilized. Caregivers often feel guilty taking time off-but it’s medically necessary. Chronic stress elevates cortisol, impairs immune function, and increases your own risk of dementia. Self-care isn’t selfish-it’s preventive medicine.
Raj Kumar
December 29, 2025 AT 21:26in india we dont have fancy blood tests but we have family who sit with them all day. no one gets lonely here. maybe we dont cure it but we dont leave them either
John Brown
December 30, 2025 AT 02:17the best thing i ever did was stop trying to make my mom remember. now i just listen to her stories-even if they’re made up. turns out, truth isn’t the point. connection is.
Michelle M
December 31, 2025 AT 02:07If memory is the architecture of identity, then Alzheimer’s doesn’t just erase rooms-it demolishes the entire house. But what if love is the foundation that remains? Maybe we don’t need to rebuild the house. Maybe we just need to sit on the rubble and sing.