QT Prolongation Risk Assessment Calculator
Assess Your Risk Factors
Risk Assessment Results
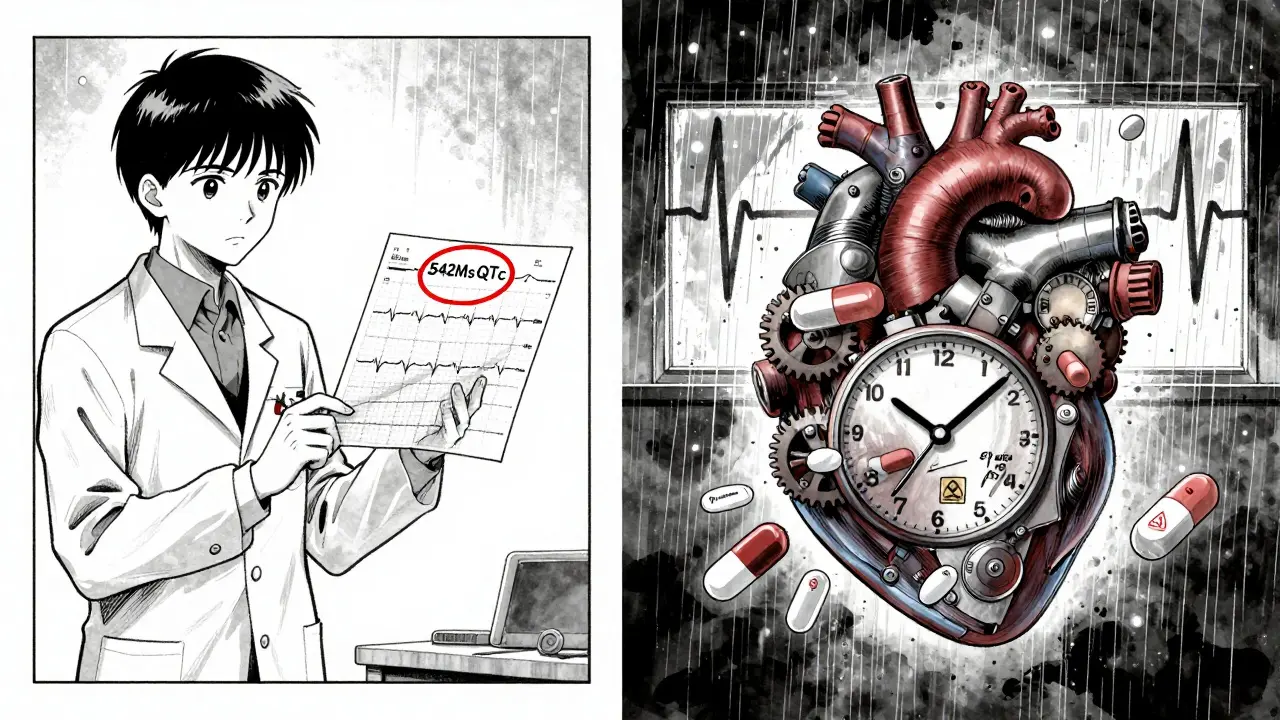
When someone is prescribed an antipsychotic for schizophrenia or severe bipolar disorder, the goal is clear: reduce hallucinations, calm agitation, and prevent crisis. But behind that benefit lies a quiet, often overlooked danger - a delay in the heart’s electrical recovery that can trigger a life-threatening rhythm called torsade de pointes. This isn’t theoretical. It’s measured in milliseconds on an ECG, tracked in hospital records, and documented in FDA warnings. The problem? Many antipsychotics - even the ones doctors reach for daily - can stretch the QT interval. And when they’re mixed with common cardiac drugs, the risk doesn’t just add up. It multiplies.
What Exactly Is QT Prolongation?
The QT interval on an ECG shows how long it takes the heart’s lower chambers to recharge between beats. If that recharge takes too long, the heart can misfire. That’s QT prolongation. It doesn’t cause symptoms on its own. But it sets the stage for torsade de pointes - a chaotic, fast heartbeat that can collapse into sudden cardiac arrest. The threshold for concern? A corrected QT interval (QTc) over 500 milliseconds. An increase of more than 60 ms from baseline also triggers action. For men, QTc above 450 ms is a red flag. For women, it’s 470 ms. These aren’t arbitrary numbers. They’re based on decades of data linking prolonged intervals to sudden death.
What makes this tricky is that many people don’t know they’re at risk until it’s too late. A 2023 study of 1,200 psychiatric inpatients found nearly 1 in 5 developed a QTc over 500 ms while on antipsychotics. And in two-thirds of those cases, they were also taking another medication that stretched the QT interval - like a diuretic, an antibiotic, or a heart rhythm drug. It’s not just the antipsychotic. It’s the combo.
Which Antipsychotics Carry the Highest Risk?
Not all antipsychotics are equal when it comes to heart risk. The difference isn’t subtle - it’s dramatic.
Thioridazine, pulled from the U.S. market in 2005, could lengthen the QT interval by up to 35 milliseconds. That’s the highest on record. Haloperidol, still widely used, adds 4-6 ms. Olanzapine? Same range. But ziprasidone? It pushes QTc up by 10-15 ms - enough to earn a black box warning from the FDA. Then there’s lurasidone, which barely moves the needle - just 1-2 ms. That’s why it’s increasingly the go-to choice for patients with heart disease or multiple risk factors.
Here’s how the risk breaks down, based on CredibleMeds and recent pharmacovigilance data:
- High risk: Thioridazine (withdrawn), haloperidol, ziprasidone
- Moderate risk: Quetiapine, risperidone, iloperidone
- Low risk: Aripiprazole, brexpiprazole, lurasidone, paliperidone
The 2023 FDA Adverse Event Reporting System analysis showed ziprasidone had a reporting odds ratio (ROR) of 4.9 for QT prolongation - meaning it was nearly five times more likely to be linked to this issue than average. Haloperidol was at 5.8. Lurasidone? Just 1.2 - almost background noise. That’s not a typo. It’s data.
Cardiac Medications That Make It Worse
It’s not just antipsychotics. Many heart drugs do the same thing. When you stack them, the effect isn’t linear - it’s exponential.
Common cardiac medications that prolong QT include:
- Amiodarone (used for atrial fibrillation)
- Quinidine and procainamide (old-school antiarrhythmics)
- Macrolide antibiotics like azithromycin
- Fluoroquinolones like moxifloxacin
- Diuretics that cause low potassium or magnesium
Here’s the real-world impact: 63% of documented QT prolongation cases involve two or more QT-prolonging drugs. A patient on haloperidol for psychosis, who also takes furosemide for fluid retention and azithromycin for a chest infection? That’s a perfect storm. The heart’s repolarization gets hit from three sides. And the body’s electrolytes - potassium, magnesium - get drained by the diuretic. That’s when torsade becomes a real possibility.
One case from Massachusetts General Hospital involved a 72-year-old woman on risperidone and hydrochlorothiazide. Her QTc jumped from 440 ms to 542 ms in 10 days. She had no symptoms. No dizziness. No fainting. But her ECG told the story. Stopping the diuretic and switching to lurasidone brought her QTc back to normal within two weeks.
Who’s Most at Risk?
Some people are walking time bombs - even before they start an antipsychotic.
Key risk factors include:
- Age over 65 (2.3 times higher risk)
- Female sex (1.7 times higher risk)
- Low potassium (<3.5 mmol/L) or low magnesium (<1.8 mg/dL)
- Heart failure or prior heart attack
- Genetic conditions like long QT syndrome
- High doses of antipsychotics
- Combining multiple QT-prolonging drugs
It’s not just about the drug. It’s about the person. A 68-year-old woman with diabetes, on a low-dose antipsychotic, who’s also taking a statin and a diuretic? She’s in the danger zone. A 30-year-old man with no medical history, on lurasidone, with normal electrolytes? His risk is minimal.
Studies show that 41% of clinicians have withheld an antipsychotic because the patient’s QTc was borderline. That’s not overcaution - it’s survival. The alternative? A sudden death in a psychiatric ward that could’ve been prevented with a simple ECG.
What Should Doctors Do?
Guidelines from the British Heart Rhythm Society and the Maudsley Prescribing Guidelines are clear: monitor, don’t guess.
Here’s the practical protocol:
- Baseline ECG: Before starting any antipsychotic, get an ECG. Don’t skip this, even if the patient seems healthy.
- Repeat ECG: Within one week of reaching a stable dose - especially for high or moderate-risk drugs.
- Check electrolytes: Potassium above 4.0 mmol/L, magnesium above 1.8 mg/dL. Fix abnormalities before or while starting the drug.
- Review all meds: Ask about antibiotics, heart drugs, antifungals, even over-the-counter cold remedies. Many contain QT-prolonging ingredients.
- Choose wisely: For patients with heart disease, older age, or multiple meds, start with lurasidone, aripiprazole, or brexpiprazole. Avoid haloperidol and ziprasidone unless absolutely necessary.
- Annual monitoring: Even if the first ECG is normal, repeat it yearly - especially if doses change or new drugs are added.
And here’s the hard truth: 68% of non-cardiologists misread QT intervals without training. A doctor might think a 490 ms QTc is fine. But if it’s 60 ms above baseline? That’s a red flag. That’s why ECG interpretation training is no longer optional - it’s essential.

Can You Avoid Antipsychotics Altogether?
Some clinicians wonder: if the risk is this high, should we just avoid antipsychotics? The answer is no - and here’s why.
People with schizophrenia have a 5% lifetime risk of suicide. They’re 12% more likely to die from accidents. Their overall mortality is 2-3 times higher than the general population. But here’s the key finding: those taking antipsychotics have 40% lower mortality than those who don’t. That’s not a small benefit. That’s life-saving.
The risk follows a U-shaped curve. People who take no antipsychotics die more. People on the highest doses die more. But those on low-to-moderate doses? They live longer. The goal isn’t to avoid the drug. It’s to use it safely.
As one expert put it: "Assume all antipsychotics carry an increased risk of sudden cardiac death. But they also protect against the consequences of schizophrenia."
What’s Changing Now?
The landscape is shifting fast.
Since 2005, the FDA has required all new antipsychotics to undergo a "thorough QT" study - testing in over 100 healthy volunteers to measure exact QT effects before approval. Three drug candidates were rejected between 2015 and 2020 because they stretched the QT interval too much. That’s not common. It’s rare. And it shows regulators are serious.
Meanwhile, prescribing patterns are changing. Sales of lurasidone rose 14.2% in 2022. Sales of haloperidol fell 3.7%. Why? Because doctors are learning. Hospitals are updating formularies. Sixty-three percent of U.S. academic medical centers now have QT risk-based prescribing rules. Telemedicine ECGs are making monitoring easier in community clinics. By 2026, ECG monitoring for antipsychotic users is expected to rise 22%.
The message is clear: cardiac safety isn’t a side note. It’s part of the prescription.
Final Takeaway: Monitor, Don’t Fear
Antipsychotics save lives. But they can also stop them - if you ignore the heart. The solution isn’t to stop using them. It’s to use them smarter.
Get the ECG. Check the potassium. Review every other drug. Choose the lowest-risk option when you can. And never assume a patient is "too healthy" to need monitoring. The heart doesn’t care if you’re 25 or 75. It just responds to the electrical signals it gets.
One ECG. One blood test. One conversation about other meds. That’s all it takes to prevent a death that no one saw coming.


Akshaya Gandra _ Student - EastCaryMS
January 3, 2026 AT 16:46so i was on risperidone for a bit and my doc never checked my ekg 😳 like how is this not standard?? i had no symptoms but my potassium was low af from drinking too much coffee and eating junk food. why dont they just test everyone??
Jacob Milano
January 4, 2026 AT 21:27Man, this post is a godsend. I’ve seen too many patients get shuffled through the system like they’re just a checklist item - ‘antipsychotic? check. ECG? nah, they’re fine.’ The fact that QT prolongation can sneak up silent as a ghost, then drop you like a stone… it’s terrifying. Lurasidone should be the new first-line for anyone with a heartbeat and a history of meds. And yeah, azithromycin + haloperidol? That’s not a prescription. That’s a death wish wrapped in a pharmacy bag. Someone needs to slap a warning label on every antibiotic script when the patient’s on an antipsychotic. Like, literally. ‘Caution: This could stop your heart.’
Shanna Sung
January 6, 2026 AT 18:01they dont want you to know this but the pharmaceutical companies pay off the FDA and the cardiologists and the whole system is rigged to keep you on the expensive drugs that make the most money even if they kill you and the low risk ones like lurasidone are hidden because theyre generic and dont make enough profit and your doctor is just a puppet
Joseph Snow
January 8, 2026 AT 10:31The assertion that lurasidone is ‘low risk’ is statistically misleading. The sample sizes in pharmacovigilance databases are inherently biased. Moreover, QT prolongation is a multifactorial phenomenon influenced by genetic polymorphisms in hERG channels, which are not accounted for in population-level data. To claim that any antipsychotic is ‘safe’ without individualized genotyping is reckless. Furthermore, the FDA’s ROR metric is notoriously prone to confounding by indication. This article reads like a marketing brochure for Sun Pharma.
melissa cucic
January 8, 2026 AT 18:44Thank you for sharing this with such clarity. I’ve been working in psych ward nursing for over a decade, and I’ve seen the consequences firsthand - the silent ECGs, the missed potassium levels, the patients who collapse without warning. This isn’t just about drugs; it’s about systems. We need mandatory baseline and follow-up ECGs for anyone on QT-prolonging meds, especially in inpatient settings. And we need better communication between psychiatry and cardiology - they’re not separate silos. The heart doesn’t care if you’re seeing a shrink or a cardiologist. It just wants to beat safely. Let’s start treating the whole person.
Dee Humprey
January 10, 2026 AT 03:16My mom was on haloperidol + furosemide for years. No one ever checked her QT. She had a near-miss in 2021 - passed out in the kitchen, no warning. They found her QTc at 560. Switched to aripiprazole, added potassium, and she’s been fine since. 🙏 Don’t wait for collapse. Ask for the ECG. Ask about alternatives. You’ve got rights.
John Wilmerding
January 11, 2026 AT 06:16While the clinical data presented is robust and aligns with current guidelines from the American Heart Association and the American Psychiatric Association, I would like to emphasize the importance of therapeutic drug monitoring in conjunction with electrocardiographic surveillance. Additionally, clinicians should consider baseline electrolyte panels, renal function tests, and concomitant medication reviews prior to initiating any antipsychotic regimen with known QT-prolonging potential. Proactive risk mitigation is not merely prudent - it is ethically imperative.
Siobhan Goggin
January 11, 2026 AT 17:00This is why I always tell my friends to ask their doctors: ‘What’s the safest option for my heart?’ Not the cheapest. Not the most popular. The safest. 💪