Living with celiac disease isn’t just about avoiding bread or pasta. It’s about rebuilding your body from the inside out. When you have celiac disease, your immune system attacks your small intestine every time you eat gluten - even a tiny crumb. That damage stops your body from absorbing nutrients properly. Without treatment, you risk serious problems like anemia, weak bones, nerve damage, and even rare cancers. The good news? Strictly going gluten-free heals your gut in most cases - and fixing nutrient gaps can turn your energy, mood, and health around.
What Exactly Happens When You Eat Gluten With Celiac Disease?
Gluten is a protein found in wheat, barley, rye, and their cousins like spelt and triticale. For someone with celiac disease, gluten triggers an autoimmune reaction. Your immune system doesn’t just react to gluten - it mistakes your own intestinal lining for a threat. This causes inflammation, flattens the tiny finger-like projections (villi) in your small intestine, and shuts down nutrient absorption. You might not even feel sick right away. Some people have severe diarrhea and weight loss. Others feel tired, get brain fog, or have joint pain. A surprising number have no digestive symptoms at all - just low iron or vitamin D.
That’s why diagnosis is tricky. The standard blood test checks for tissue transglutaminase antibodies (tTG-IgA). It’s 98% accurate - but only if you’re still eating gluten. If you’ve already cut it out, the test can look normal even if you have celiac. That’s why doctors stress: don’t start a gluten-free diet before testing. The gold standard is still an endoscopy with biopsy, though new guidelines now allow diagnosis in children without a biopsy if antibody levels are very high and other criteria are met.
The Gluten-Free Diet: What You Can and Can’t Eat
Going gluten-free sounds simple until you realize how many hidden sources there are. Gluten isn’t just in bread. It’s in soy sauce, salad dressings, soups, processed meats, even some medications and supplements. Labels say “wheat-free,” but that doesn’t mean gluten-free. You need to look for “certified gluten-free” - which means the product has been tested to contain less than 20 parts per million (ppm) of gluten, the safety threshold set by the FDA and European regulators.
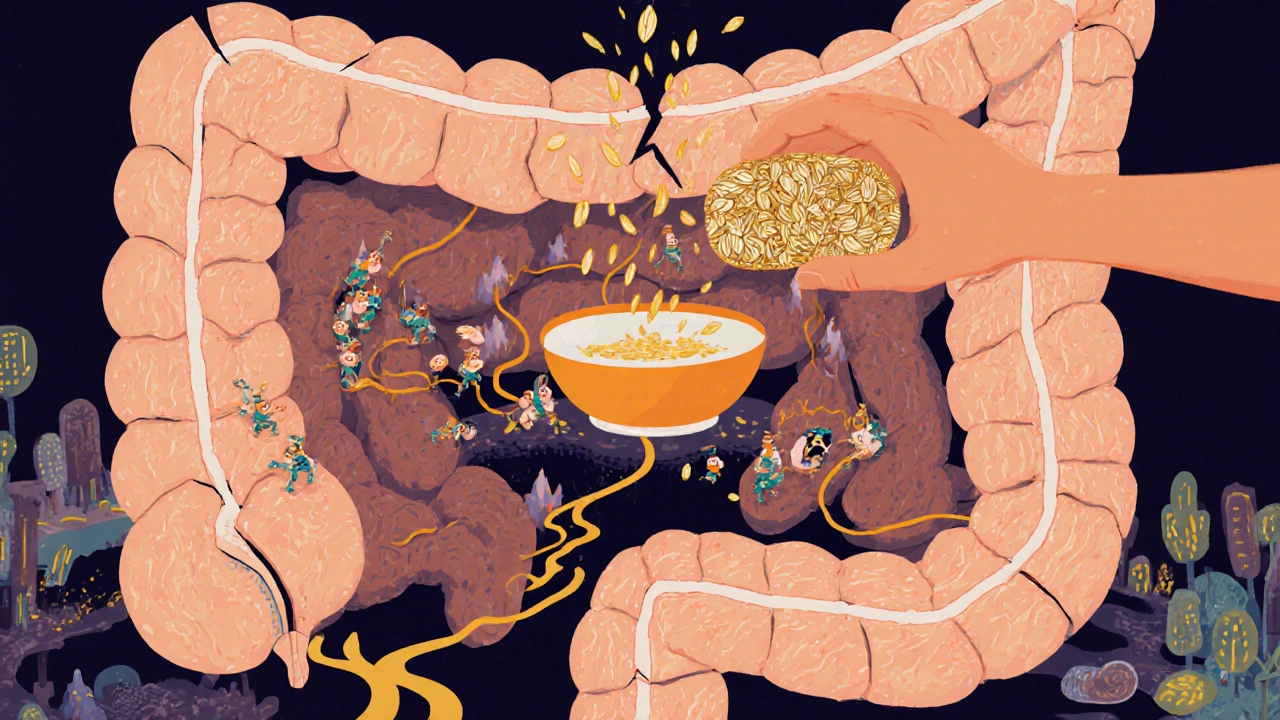
Safe grains include rice, quinoa, buckwheat, millet, amaranth, sorghum, teff, and certified gluten-free oats. Yes, oats are okay - but only if they’re labeled gluten-free. Regular oats are often cross-contaminated during farming or processing. About 95% of people with celiac can safely eat up to 50 grams (about half a cup) of certified gluten-free oats per day. The other 5% still react - so start slow and watch for symptoms.
Even with clean ingredients, cross-contamination is the biggest problem. Using the same toaster for gluten-free and regular bread? A shared cutting board? A spoon used in regular pasta then dipped in gluten-free sauce? These tiny exposures add up. For many, that’s why symptoms don’t go away - even after going gluten-free. Dedicated kitchen tools, separate condiment jars, and asking restaurants about their gluten protocols are non-negotiable.
Why Nutrient Deficiencies Are Common - and Dangerous
Your damaged gut can’t absorb nutrients like it should. That’s why almost everyone with newly diagnosed celiac has at least one deficiency. Iron deficiency anemia affects 12% to 63% of patients at diagnosis. Vitamin D levels are low in 37% to 75%. Calcium is missing in 25% to 40%. Folate, B12, zinc, and magnesium are also commonly low.
These aren’t just inconveniences. Low iron means fatigue, weakness, and shortness of breath. Low vitamin D and calcium lead to osteoporosis - and broken bones can happen even in young adults. Low B12 can cause nerve damage, tingling in hands and feet, or even memory problems. Magnesium deficiency can trigger muscle cramps, anxiety, and sleep issues.
Here’s what most people need to supplement - based on clinical guidelines and real patient data:
- Iron: 18 mg daily for women, 8 mg for men - often in ferrous sulfate or bisglycinate form for better absorption
- Vitamin D: 600-800 IU daily, but many need 2,000-5,000 IU to correct deficiency
- Calcium: 1,000-1,200 mg daily, ideally split into two doses with meals
- Folate (B9): 400 mcg daily - avoid folic acid if you have MTHFR gene variants; use methylfolate instead
- Vitamin B12: 250-500 mcg daily, or 1,000 mcg sublingual (under the tongue) if absorption is poor
- Magnesium: 400 mg daily, preferably as glycinate or citrate
Don’t just guess. Get blood tests before and after starting supplements. Some people need IV iron if oral doesn’t work. Others need higher doses of vitamin D for months to reach normal levels. Your doctor or dietitian should guide this.
Why Some People Still Feel Sick After Going Gluten-Free
If you’re doing everything right - no gluten, taking supplements - but you still feel awful, you’re not alone. About 30% of people with celiac continue to have symptoms even after a year on a gluten-free diet. The most common reason? Hidden gluten.
It’s not always about eating bread. It’s about:
- Restaurant food cooked on the same grill as regular items
- Shared fryers (French fries, chicken nuggets)
- Medications with gluten as a filler (about 30% of prescriptions contain it)
- Beauty products like lip balm or toothpaste that you swallow
- “Gluten-free” snacks that still contain 15-19 ppm - enough to keep your gut inflamed
Some people also have another condition - like small intestinal bacterial overgrowth (SIBO), lactose intolerance, or fructose malabsorption - that develops after celiac damage. Others have a second autoimmune disorder, like thyroid disease, which needs separate treatment.
Doctors now recommend a follow-up plan: blood tests at 3 and 6 months, then yearly. A DXA scan for bone density every 2-3 years. If symptoms persist, a capsule endoscopy can check if your gut has truly healed. The goal isn’t just symptom relief - it’s full mucosal recovery. Only 40-60% of adults achieve this within two years, even with perfect diets.

Practical Tips for Real-Life Gluten-Free Living
Living gluten-free is easier than it was 10 years ago - but still hard. Grocery stores now have 350% more gluten-free products than in 2015. Still, they cost up to 159% more. A loaf of gluten-free bread can be $5.99; regular bread is $2.31. That’s a financial burden.
Here’s how to make it manageable:
- Focus on whole foods: Fruits, vegetables, eggs, meat, fish, beans, rice, and certified gluten-free oats are naturally safe and cheaper than packaged substitutes.
- Use apps: The Nima Sensor (2024 model) tests food for gluten in minutes - accurate at 20 ppm. The Gluten-Free Drug Database by the University of Chicago tells you if your pills are safe.
- Carry restaurant cards: The Celiac Disease Foundation offers free cards in 30+ languages explaining your needs in simple terms.
- Get a dietitian: Only 78% of U.S. hospitals have certified gluten-free dietitians - but they’re worth it. They help you avoid hidden traps and tailor supplements to your needs.
- Check your supplements: Many multivitamins and probiotics contain gluten as a filler. Look for “certified gluten-free” on the label.
Don’t wait six months to get help. Start with a blood test, then see a dietitian within the first month. Most people feel better in days - but full healing takes months or years.
What’s Next for Celiac Disease?
There’s no cure yet - but research is moving fast. Enzyme therapies like Latiglutenase are in Phase 3 trials and may help protect against accidental gluten exposure. A vaccine (Nexvax2) is being tested, but early results were disappointing. Non-invasive tests like epithelial lymphogram analysis - which looks at immune cells in the gut lining - are now being used in Europe and could replace biopsies in the future.
For now, the best tool is still a strict gluten-free diet - paired with smart supplementation. People who stick with it have near-normal life expectancy. Those who don’t face a 2.5 times higher risk of early death.
You don’t have to be perfect. But you do need to be consistent. Every crumb matters. Every supplement counts. And healing - real, deep healing - is possible.
Can you outgrow celiac disease?
No. Celiac disease is a lifelong autoimmune condition. Once diagnosed, you must avoid gluten forever. Even small amounts can trigger damage, even if you don’t feel symptoms. There’s no cure, and no evidence that the immune system ever stops reacting to gluten.
Are oats safe for people with celiac disease?
Certified gluten-free oats are safe for about 95% of people with celiac disease. The key is certification - regular oats are almost always contaminated with wheat during farming or processing. Start with small amounts (50g per day) and watch for symptoms. If you develop bloating, fatigue, or diarrhea after eating oats, stop and talk to your doctor. About 5% of people still react, even to certified oats.
Why do I still feel tired after going gluten-free?
Fatigue often lingers because nutrient deficiencies take time to correct. Low iron, vitamin D, B12, or magnesium can cause chronic tiredness. Even after starting supplements, it can take 3-6 months for your body to rebuild its stores. If you’re still tired after a year, get blood tests again. You might need IV iron, higher doses of vitamin D, or to check for other issues like thyroid disease or SIBO.
Can I drink alcohol with celiac disease?
Yes - but only certain types. Distilled spirits like vodka, gin, whiskey, and rum are gluten-free because the distillation process removes gluten proteins. Wine and hard ciders are also safe. Beer, malt liquor, and most ales contain barley and are not safe unless labeled gluten-free. Some gluten-free beers are made from sorghum or rice. Always check labels - some “gluten-removed” beers aren’t reliable for people with celiac.
Do I need to take supplements forever?
Not necessarily. Most people only need supplements for 6-18 months while their gut heals and nutrient levels normalize. After that, you may be able to get everything from food - if your diet is balanced and varied. But some people, especially those with severe initial deficiencies or ongoing absorption issues, need to continue supplements long-term. Get blood tests every year to know for sure.
Stick with it. Your gut will heal. Your energy will return. And you’ll find that life without gluten isn’t a limitation - it’s a new way of eating that puts your health first.


Andrew Forthmuller
November 13, 2025 AT 20:04Just went gluten-free last month and my brain fog lifted in 3 days. No joke.
Elizabeth Buján
November 14, 2025 AT 13:31I was diagnosed 5 years ago and honestly? The worst part wasn’t the food-it was the loneliness. People think it’s a trend, like you’re just picky. But when you’re the one crying in the grocery store because you can’t find a safe muffin, you realize this isn’t a diet. It’s a lifestyle overhaul. And yeah, the supplements? Life-changing. I was so tired I’d nap after brushing my teeth. Now I hike on weekends. It took time, but healing isn’t linear. Just keep going. You’re not broken-you’re rebuilding.
vanessa k
November 16, 2025 AT 00:33My sister has celiac and she still gets sick sometimes. I thought she was just being dramatic until I learned about cross-contamination. Now I have a separate toaster, separate cutting board, and I even wash my hands before handling her food. It’s annoying, but if it keeps her alive, it’s worth it. No one talks about how much emotional labor this takes. You’re not just avoiding gluten-you’re avoiding judgment, confusion, and bad intentions from people who just don’t get it.
manish kumar
November 18, 2025 AT 00:25As someone from India where wheat is practically a religion, going gluten-free was a cultural earthquake. Rotis, parathas, naan-gone. But here’s the thing: traditional Indian diets are full of naturally gluten-free staples like rice, lentils, millets like ragi and jowar, and even some fermented foods like idli and dosa (if made with rice and lentils). I started cooking more at home, switched to certified gluten-free soy sauce (shoyu), and found that many Ayurvedic herbs like ashwagandha and turmeric actually help gut healing. It’s not just about removing gluten-it’s about rebuilding with what your body already knows. Also, I started taking magnesium glycinate and my sleep improved so much I cried. Seriously. Sleep is the unsung hero of recovery.
Nicole M
November 18, 2025 AT 15:24Anyone else notice that gluten-free bread tastes like cardboard but costs 3x more? I just eat rice cakes with avocado and eggs. So much easier. And yes, I checked my multivitamin-gluten-free label. Learned that the hard way after a month of zero improvement.
Arpita Shukla
November 20, 2025 AT 00:21Actually, the FDA’s 20ppm threshold is outdated. Studies show that even 5ppm can trigger immune response in sensitive individuals. Also, many ‘gluten-free’ oats are contaminated because they’re processed in the same facilities as wheat. The real solution? Go whole foods only. No processed substitutes. No ‘gluten-free’ snacks. Just meat, veggies, fruits, nuts, rice. You don’t need gluten-free pasta to be healthy. You need to stop buying marketing.
Benjamin Stöffler
November 20, 2025 AT 16:09Let’s be clear: celiac is not a ‘diet’-it’s a life sentence. And if you think you can ‘cheat’-you’re lying to yourself. Gluten is not a suggestion. It’s a toxin. And if your doctor didn’t test you before you went gluten-free? You’re probably misdiagnosed. And if you’re still tired after supplements? You’re probably not taking enough. Or you’re taking the wrong form. Folic acid? No. Methylfolate? Yes. Ferrous sulfate? Maybe. Bisglycinate? Better. Vitamin D? 600 IU? Ha. You need 5,000. And you need to test every 6 months. Not once a year. Every. Six. Months.
Mark Rutkowski
November 21, 2025 AT 22:02There’s something sacred about healing your gut. It’s not just about avoiding bread-it’s about listening to your body in a world that screams at you to consume more, faster, cheaper. Gluten-free isn’t a restriction-it’s a rebellion against a system that treats food like a commodity. When I started eating real food-no labels, no gimmicks, just eggs, sweet potatoes, and wild salmon-I didn’t just feel better. I felt like myself again. And that’s not just health. That’s homecoming.
Ryan Everhart
November 23, 2025 AT 03:39So you’re telling me the only cure for a disease caused by eating wheat is… not eating wheat? Groundbreaking. Next you’ll tell me smoking causes lung cancer. I mean, who knew? Anyway, I’ve been gluten-free for 8 years. Still tired. Still taking supplements. Still broke from the bread prices. But hey, at least I’m not dead. So congrats? I guess?
David Barry
November 23, 2025 AT 07:54Let’s be real: 90% of people with celiac don’t follow the diet properly. They eat ‘gluten-free’ snacks with 19ppm, use the same toaster, and then blame their fatigue on ‘stress.’ Meanwhile, their villi are still flattened. And their doctors? They’re just happy you’re not eating bread. No one checks for SIBO. No one checks for thyroid. No one says, ‘Maybe you’re not healing because you’re still poisoning yourself.’ The system is broken. You’re not special. You’re just the latest person who didn’t get the full picture.
Elizabeth Buján
November 24, 2025 AT 00:56Just read your comment about the 19ppm thing. You’re right. I thought I was doing everything right-until I got a Nima sensor. Tested my ‘gluten-free’ granola bar? 17ppm. I threw it out. That’s when I realized: healing isn’t about willpower. It’s about tools. And yeah, it’s expensive. But my energy? Worth every penny. Thanks for calling it out. I’m not alone in this.