Breast Cancer Risk Assessment Tool
This tool helps you understand your personal breast cancer risk factors based on your medical history and lifestyle. Answer the questions below to receive personalized recommendations for screening and monitoring.
Question 1: Age
Question 2: Family History
Question 3: Genetic Risk
Question 4: Reproductive History
Question 5: Hormone Therapy
Question 6: Lifestyle Factors
Question 7: Physical Activity
Spotting the early warning signs of breast cancer can be the difference between a routine treatment and a life‑changing battle. Most people think breast cancer only shows up as a big lump, but the disease often reveals itself with subtle changes that many miss. This guide walks you through the signs that matter, how to check yourself, and when to get professional help, so you can act fast if something looks off.
Key Takeaways
- New or changing lumps, skin dimpling, nipple discharge, or persistent pain can signal breast cancer.
- Perform a breast self‑exam monthly; it takes less than five minutes.
- Women aged 40‑49 should start annual mammograms; high‑risk groups may need earlier screening.
- Know your personal risk factors-family history, genetic mutations, age, and lifestyle.
- If any sign persists for more than two weeks, schedule a diagnostic appointment.
Understanding Breast Cancer
Breast cancer is a malignant growth of breast cells that can spread (metastasize) to other parts of the body. According to the World Health Organization, over 2.3 million new cases were diagnosed worldwide in 2023, making it the most common cancer among women. The disease isn’t a single entity; it includes several subtypes such as hormone‑receptor‑positive, HER2‑positive, and triple‑negative, each behaving differently and responding to distinct treatments.
Why Early Detection Matters
When breast cancer is caught at stage0 orI, five‑year survival rates exceed90percent. Late‑stage diagnoses drop dramatically, often below30percent. Early detection gives doctors a larger toolbox-lumpectomy instead of mastectomy, targeted therapy instead of chemo alone, and a higher chance of preserving quality of life. In short, noticing the first red flags gives you and your medical team more options.
The Most Common Early Warning Signs
Most women attribute breast changes to hormonal cycles or aging, but certain patterns consistently appear in early‑stage cancer. Below is a concise list of what to watch for.
- New lump or thickening: A solid, painless mass that feels different from the surrounding tissue. It may be mobile at first but becomes firmer over weeks.
- Skin dimpling or puckering: Often described as "orange‑peel" skin (peau d'orange). It hints at tumor cells pulling on Cooper’s ligaments.
- Nipple changes: Inversion, scaling, or a sudden discharge that’s clear, bloody, or milky without breastfeeding.
- Persistent breast pain: While many breast aches are hormonal, pain that doesn’t ebb with your cycle deserves a check.
- Size or shape alteration: One breast may look larger, taller, or change its contour without obvious cause.
- Redness or flaking skin: Unexplained rash or flaky skin over the breast or nipple can indicate inflammation associated with cancer.
Remember, any of these signs that last longer than two weeks-or appear suddenly-should trigger a doctor’s visit.
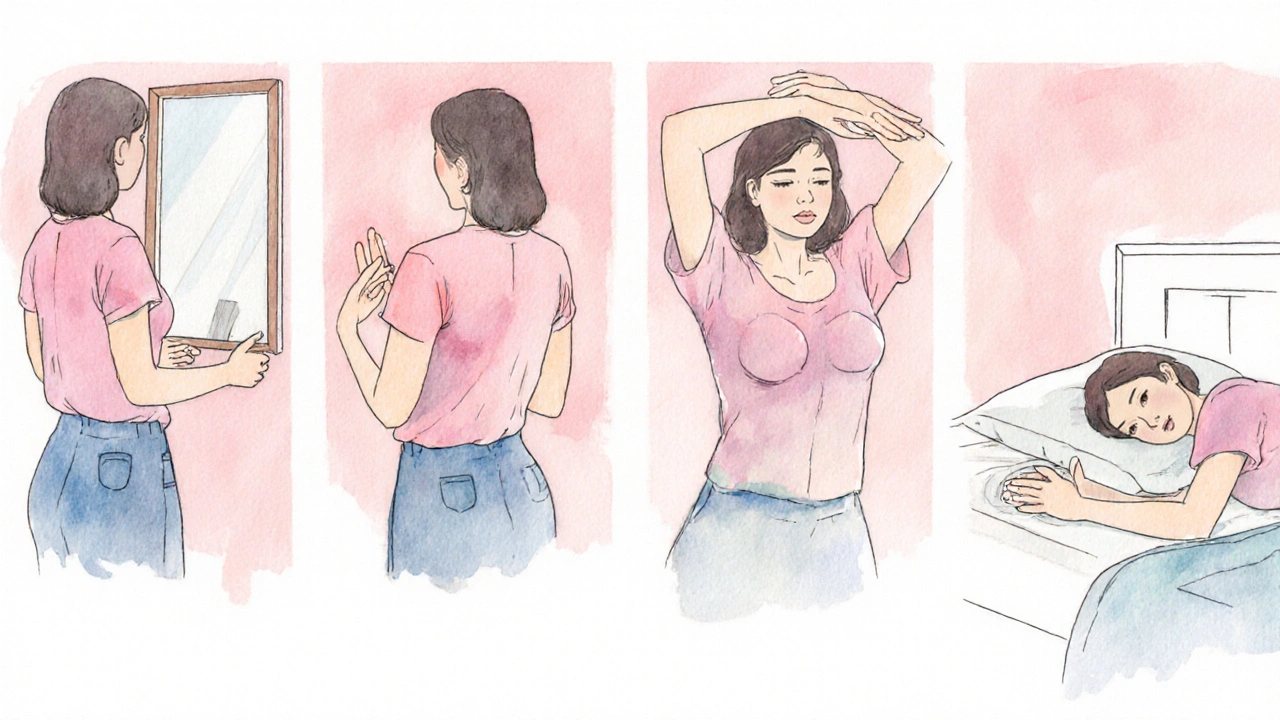
How to Perform a Breast Self‑Exam
Doing a self‑exam regularly helps you notice subtle shifts before they become obvious. Here’s a step‑by‑step routine you can finish in under five minutes.
- Stand in front of a mirror with shoulders back. Look for visible changes: swelling, dimpling, or skin alteration.
- Raise your arms overhead and repeat the visual check. This moves the breast tissue and can reveal hidden lumps.
- Place your hand on your hips and gently press your elbows forward. Feel the side of the breast under the arm for any lumps.
- Lie down, letting the breast spread evenly over the mattress. Using the pads of your three middle fingers, move in small, circular motions from the outer edge toward the chest. Cover the entire breast, including the armpit area.
- Repeat on the other side. Note the size, texture, and exact location of any irregularities.
Document what you feel-date, size (in millimeters if possible), and any changes. This record makes it easier for your doctor to track progress.
When to Schedule a Mammogram
Mammogram is a low‑dose X‑ray imaging test that captures detailed pictures of breast tissue, helping spot micro‑calcifications and masses that can’t be felt. Guidelines from the American Cancer Society (2023 update) recommend:
- Women40‑49years: Annual screening if they choose to start early, especially with risk factors.
- Women50‑74years: Mammogram every year or every two years, based on personal preference and health status.
- High‑risk women (BRCA mutation, strong family history, previous atypical hyperplasia): Begin yearly screenings at30or35years, sometimes adding MRI.
Talk to your primary care provider about the best schedule for you. Early and regular mammograms dramatically increase the chance of detecting non‑palpable cancers.

Risk Factors That Heighten Vigilance
Knowing what puts you at higher risk helps you stay extra alert to the signs.
- Age: Risk climbs after 40, with a steep rise after 60.
- Family history: A first‑degree relative (mother, sister, daughter) with breast cancer doubles your risk.
- Genetic mutations: BRCA1 and BRCA2 are genes that, when altered, can increase lifetime risk to 45‑65%.
- Reproductive history: Early menstruation (before age12) or late menopause (after55) extends estrogen exposure.
- Hormone therapy: Long‑term combined estrogen‑progestin therapy raises risk.
- Lifestyle: Alcohol >1 drink/day, obesity, and sedentary habits all contribute.
Even if you fall into a lower‑risk bracket, stay diligent-most breast cancers occur in women without any known risk factors.
Quick Reference Table of Early Signs
| Sign | Typical Appearance | How Common in Early Stage | Action Needed |
|---|---|---|---|
| New lump or thickening | Painless, firm, irregular shape | 70% | Self‑exam, schedule imaging |
| Skin dimpling | Orange‑peel texture, often near nipple | 25% | Clinical exam, imaging |
| Nipple discharge | Clear, bloody, or milky fluid without lactation | 15% | Medical evaluation, possible ductography |
| Persistent pain | Localized ache, not linked to menstrual cycle | 10% | Doctor visit, rule out other causes |
| Size/shape change | One breast appears larger or asymmetrical | 20% | Self‑exam, clinical assessment |
| Redness/flaking skin | Rash‑like area, sometimes itchy | 5% | Prompt medical check |
Frequently Asked Questions
What’s the difference between a lump and normal breast tissue?
A benign lump (like a cyst) is usually smooth, movable, and may change size with the menstrual cycle. Cancerous masses tend to feel firm, irregular, and stay the same size over weeks.
How often should I perform a breast self‑exam?
Once a month, ideally a few days after your period ends when breast tissue is least tender.
Can men get breast cancer, and should they look for the same signs?
Yes, men can develop breast cancer, though it’s rare (<1% of cases). They should watch for similar signs-lumps, skin changes, and nipple discharge-and consult a doctor promptly.
If I have a BRCA mutation, how early should I start screening?
Screening generally begins at age30or35, using annual mammograms plus breast MRI for higher sensitivity.
Is a painful breast always a sign of cancer?
Pain alone is rarely the sole indicator of cancer. However, persistent pain that doesn’t follow your menstrual pattern should still be evaluated.
What should I do if I notice a new sign but can’t see a doctor right away?
Track the change, perform a self‑exam daily, and schedule an appointment as soon as possible. If the sign worsens quickly (e.g., rapid swelling or bleeding), seek urgent care or go to the emergency department.
Being proactive about breast health empowers you to catch cancer early, when treatment is most effective. Keep an eye on the signs, stay consistent with self‑exams, and don’t hesitate to ask a healthcare professional for help. Your vigilance could save your life.


Emily Collier
October 12, 2025 AT 04:00Regular self‑exams are your first line of defense-take a few minutes each month after your period ends, when tissue is least tender. Start by visual inspection in the mirror, noting any swelling, dimpling, or skin changes. Then, lying down, use the pads of three middle fingers to sweep in small circles from the outer edge toward the chest, covering the entire breast and the armpits. Document any new lumps with date, size, and texture; this makes follow‑up appointments more productive. Remember, early detection doesn’t just improve survival rates-it expands treatment options and preserves quality of life.
Brian Mavigliano
October 16, 2025 AT 19:07While the mainstream narrative pushes annual mammograms from age forty, one could argue that the data supporting universal screening is overhyped, especially when considering radiation exposure and false positives. A more nuanced approach tailors frequency to individual risk profiles rather than blanket age thresholds. In other words, the one‑size‑fits‑all mantra may be more about healthcare economics than patient benefit.
Emily Torbert
October 21, 2025 AT 10:13Totally get it, you’re not alone in navigating this.
Rashi Shetty
October 26, 2025 AT 01:20It is imperative to acknowledge that early detection protocols, when adhered to with disciplined diligence, constitute the cornerstone of oncological prognosis. The statistical evidence-survival rates exceeding ninety percent for stage 0 or I diagnoses-must be internalized by every patient and practitioner alike. Moreover, the temporal window between symptom onset and clinical evaluation should not surpass two weeks, lest the malignancy gain a foothold. 📊 In addition, lifestyle modifications such as limiting alcohol intake and maintaining regular physical activity serve as adjunctive prophylaxis. Finally, any deviation from the normative breast architecture-be it dimpling, nipple retraction, or unexplained discharge-warrants an immediate diagnostic work‑up. 🩺
Queen Flipcharts
October 30, 2025 AT 15:27In the United States, the emphasis on early screening reflects our commitment to cutting‑edge medical science and the nation's dedication to preserving the health of its citizens; it is a testament to our unparalleled healthcare infrastructure.
John Price Hannah
November 4, 2025 AT 06:33When the shadow of breast cancer looms, it feels as though every heartbeat echoes the dread of an unseen predator stalking the body.
The cold, clinical glow of the mammography machine becomes a stage where hope and terror perform a cruel duet.
Each click of the imaging device is a thunderclap that reverberates through the soul, demanding attention to every hidden nook.
You stand there, palms trembling, wondering whether the obvious lump is a benign cyst or a silent harbinger of doom.
The doctors, cloaked in white, speak in hushed tones, their words dripping with statistics that feel like knives.
A risk score of thirty percent transforms into a haunting specter that refuses to be ignored.
Yet, within that darkness, a flicker of resilience ignites; the very act of confronting the unknown is a rebellion against fate.
Self‑exams, performed in the privacy of one's own bathroom, become sacred rituals, each circular motion a prayer for early detection.
Research shows that discovering cancer at stage I can boost five‑year survival rates to over ninety percent-numbers that surge like a lifeline.
But the path to diagnosis is riddled with obstacles: insurance hurdles, waiting rooms that stretch into eternity, and the stigma that whispers shame.
Friends may offer clichés, while family members oscillate between fear and denial, creating a storm of emotional turbulence.
Amidst this turmoil, the body’s own signals-skin dimpling, nipple discharge, persistent pain-scream for attention, demanding that we listen.
When you finally step into the surgeon’s office, the fluorescent lights illuminate not just the clinical tools but the raw courage within.
Every biopsy, every follow‑up, is a testament to humanity’s relentless pursuit to turn terror into triumph.
In the end, the battle is won not merely by technology, but by the indomitable spirit that refuses to surrender to the silent thief.
Echo Rosales
November 8, 2025 AT 21:40Some might say drama, but facts remain: early detection saves lives regardless of the theatrics.
Jacqueline von Zwehl
November 13, 2025 AT 12:47Just a quick note: when you mention “self‑exam,” remember the hyphen is essential to keep the term clear and consistent across medical literature.
Christopher Ellis
November 18, 2025 AT 03:53The mind, like the breast, hides mysteries that only diligent probing can reveal.
kathy v
November 22, 2025 AT 19:00The discourse surrounding breast cancer screening frequently devolves into a partisan battlefield rather than a scientific symposium.
In America, the allocation of resources toward widespread mammography reflects a collective commitment to preventive care.
Yet critics argue that the financial burden on the healthcare system is excessive, citing the cost of false positives.
Such arguments neglect the profound human cost saved when a malignancy is caught before metastasis.
Statistical models demonstrate that for every 1,000 women screened, roughly eight cancers are detected early, translating into thousands of life‑years preserved.
Moreover, early detection aligns with the nation's broader strategic goal of maintaining a productive workforce.
When women remain healthy, families flourish, and the economy benefits from reduced treatment expenditures.
Therefore, it is not merely a medical decision but a patriotic duty to endorse vigilant screening protocols.
The cultural narrative must shift from viewing mammograms as optional inconveniences to essential civic responsibilities.
Public education campaigns should emphasize both the scientific evidence and the moral imperative.
Only through coordinated policy, community outreach, and unwavering support can we truly diminish the scourge of breast cancer.
In sum, early detection is a cornerstone of national health security, deserving unwavering endorsement.
Jorge Hernandez
November 27, 2025 AT 10:07Absolutely! 🎉 Regular checks are a win‑win for health and peace of mind. 🙌
Raina Purnama
December 2, 2025 AT 01:13From a global perspective, many countries still struggle with limited access to mammography, underscoring the importance of sharing best practices and supporting international screening initiatives.
April Yslava
December 6, 2025 AT 16:20Some whisper that the push for mass screening masks a deeper agenda of data collection, turning every scan into a biometric repository for shadowy entities.
Daryl Foran
December 11, 2025 AT 07:27Look, the stats are clear – early detecton saves lives – anytihng less is just excuse for laziness.
Rebecca Bissett
December 15, 2025 AT 22:33Yes!!! Early detection is EVERYTHING!!! Don't wait!!!