Imagine taking a pill for your depression, and within an hour, you feel a wave of calm. But by mid-afternoon, that feeling fades-so you take another. Then another. You don’t realize you’ve just doubled your dose. This isn’t rare. It happens every day because people don’t understand the difference between extended-release and immediate-release medications. And the consequences can be serious-sometimes deadly.
How These Two Types Work
Immediate-release (IR) pills are the classic kind you’ve seen your whole life. They dissolve fast in your stomach. The drug hits your bloodstream in 15 to 30 minutes, peaks around 30 to 90 minutes later, and wears off in 4 to 8 hours. That’s why you might need to take IR painkillers or ADHD meds three or four times a day. Extended-release (ER, XR, SR, CR) pills are engineered differently. They don’t dump everything at once. Instead, they release the drug slowly over 12 to 24 hours. Some use a gel-like matrix that swells and lets the medicine leak out gradually. Others use tiny osmotic pumps-like a slow drip system inside the pill-that push the drug out over time. Concerta, for example, uses an osmotic pump to deliver methylphenidate evenly all day. The goal? Keep drug levels steady. With IR, your blood levels spike high, then crash. With ER, you stay in the therapeutic range-enough to work, not so much that it causes side effects. Studies show ER formulations cut peak-to-trough ratios from 3:1 in IR down to 1.5:1. That’s why bupropion ER can be taken once daily at 300mg, while IR versions can’t go above 150mg without raising seizure risk.When ER Is the Better Choice
If you’re on a daily medication for a chronic condition, ER is often the smarter option. Take hypertension. A 2022 JAMA study followed 15,000 patients on blood pressure meds. Those on ER versions had a 22% higher adherence rate. Why? Because they only had to take one pill a day instead of two or three. No forgetting lunchtime doses. No juggling schedules. Same goes for antidepressants. Over 68% of new prescriptions for SSRIs like sertraline are now ER. Why? Stable levels mean fewer mood swings, less nausea, and fewer nighttime awakenings. Quetiapine XR, for example, causes less insomnia than its IR version because the drug doesn’t spike suddenly before bed. For ADHD, Adderall XR gives 10 to 12 hours of symptom control. Adderall IR lasts only 5 to 8. That means kids on IR often need a midday dose at school-something many parents and teachers find awkward or logistically impossible. ER eliminates that.Why IR Still Matters
Don’t write off immediate-release. It’s not outdated-it’s essential in the right situations. Think about pain. If you’re having a sudden flare-up, you need relief now. ER opioids take 2 to 4 hours to kick in. That’s too long when you’re in acute pain. IR morphine or oxycodone? It hits fast. Same with anxiety-someone having a panic attack doesn’t want to wait 4 hours for a pill to work. IR benzodiazepines like alprazolam are used for that exact reason. Also, IR is critical for titration. When a doctor starts you on a new medication, they need to find the right dose. With IR, they can adjust in small steps each day. With ER, you’re stuck with whatever dose you’re on for a full day. That’s why new prescriptions for antidepressants or mood stabilizers often start as IR before switching to ER.
The Hidden Dangers of ER
ER sounds safer because you take less often. But it’s riskier if you don’t know how to use it. The biggest danger? Crushing, chewing, or splitting ER pills. Over 92% of extended-release formulations are designed to be swallowed whole. Break them open, and you release the entire dose at once. That’s like injecting a time-release drug directly into your bloodstream. The FDA issued a safety alert in 2020 warning that crushing ER opioids can cause fatal overdoses. But it’s not just opioids. Take venlafaxine XR-some patients split it to save money. That’s dangerous. The coating is broken, and you get a sudden surge of serotonin. Same with bupropion: crushing an ER tablet can send plasma levels over 350 ng/mL-the threshold where seizures become likely. Another risk? Delayed onset. People don’t realize ER meds take 2 to 4 hours to even start working. If you don’t feel better after an hour, you might take another. That’s how accidental overdoses happen. A 2022 GoodRx survey found 41% of ER users initially thought the drug wasn’t working-and 28% took extra doses. Nine percent ended up with adverse events. And if you have gastroparesis-a condition where your stomach empties slowly-ER meds can behave unpredictably. The FDA warned in 2023 that patients with this condition can absorb 30% to 50% more drug than normal, leading to toxic levels. Your body doesn’t process the slow-release mechanism the way it should.Cost, Convenience, and Compliance
ER versions cost 15% to 25% more than IR. Adderall XR runs $350-$450 for 30 capsules. Adderall IR? $280-$380. That gap matters, especially without good insurance. But here’s the twist: even though ER costs more upfront, it saves money long-term. Higher adherence means fewer hospital visits, ER trips, and missed workdays. The JAMA study showed ER users had fewer complications overall. For chronic conditions, the savings add up. And let’s talk about real life. A Reddit user on r/ADHD said: “I use XR for work, but I keep 5mg IR tabs for when I need instant focus before a presentation.” That’s smart. It’s not all or nothing. Many people use a combination-ER for baseline control, IR for breakthrough symptoms.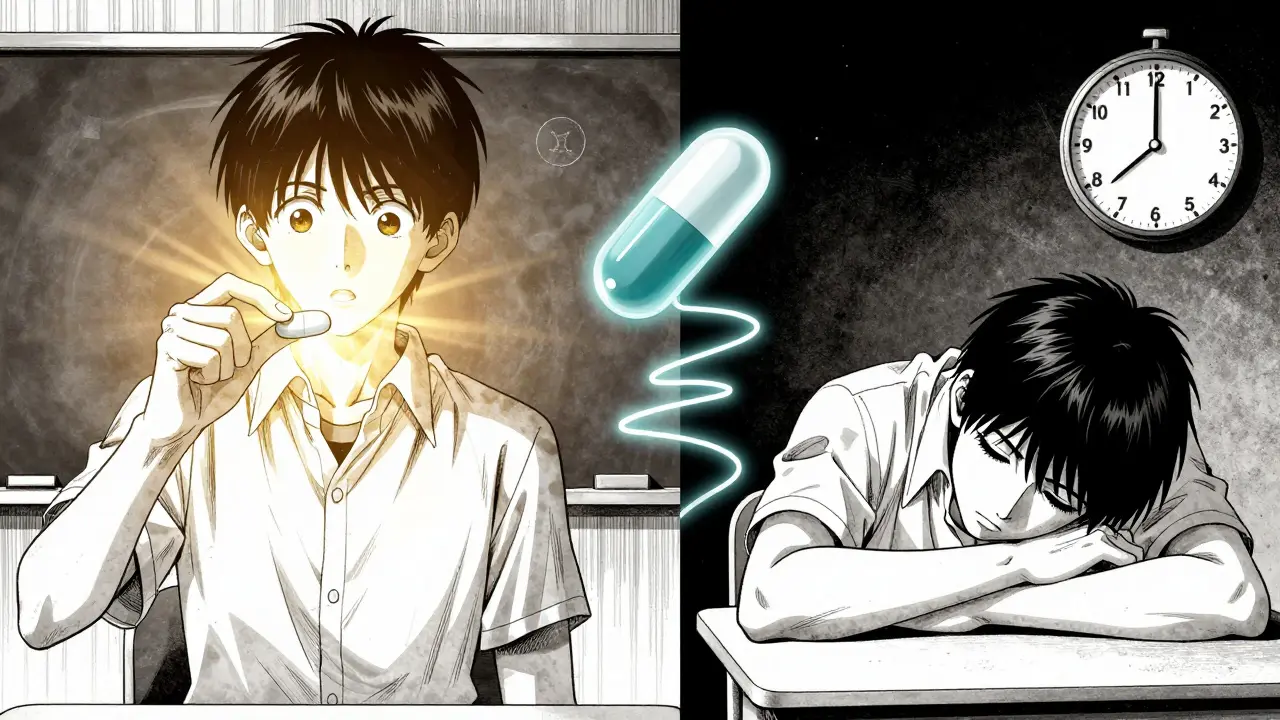
What You Should Do
If you’re prescribed an ER medication:- Never crush, split, or chew it-unless your doctor or pharmacist specifically says it’s safe.
- Wait at least 2 to 4 hours before deciding it’s not working. It takes time to build up.
- Don’t take an extra dose because you “feel nothing.” That’s how overdoses start.
- Ask your pharmacist: “Is this tablet scored? Can it be split?” Many ER pills aren’t.
- If you have digestive issues like gastroparesis, tell your doctor. ER meds may not be right for you.
- Set phone alarms for doses. Missing one can cause withdrawal or rebound symptoms.
- Keep a small supply of extra pills if you travel or have unpredictable days.
- Use IR for acute symptoms, not daily maintenance.
What’s Next for Medication Delivery
The future is getting smarter. Companies are developing abuse-deterrent ER tech-like pills that turn into gel when crushed, making them impossible to snort. MIT researchers are even 3D-printing “polypills” that release different drugs at precise times-perfect for people on five or six meds a day. But for now, the most important thing isn’t the technology. It’s understanding what’s in your pill bottle. You wouldn’t drive a car without knowing how the brakes work. Don’t take medication without knowing how it releases. Your body doesn’t know the difference between a pill and a timed bomb-if you mess with the timing, you’re the one who pays the price.Can I split an extended-release pill in half to save money?
No-unless the pill is specifically scored and labeled as safe to split. Most extended-release tablets have special coatings or matrices that control drug release. Splitting them destroys that mechanism and can cause a dangerous rush of medication into your system. For example, splitting venlafaxine XR or bupropion XL can lead to overdose, seizures, or severe side effects. Always check with your pharmacist before cutting any pill.
Why does my ER medication take so long to work?
Extended-release pills are designed to release medication slowly over 12 to 24 hours. That means it can take 2 to 4 hours just to reach detectable levels in your blood. Full effect may take days or even weeks, especially for antidepressants or mood stabilizers. This is normal. Taking extra doses because you don’t feel immediate results can lead to dangerous overdose. Give it time.
Is extended-release always better than immediate-release?
No. ER is better for daily maintenance of chronic conditions like depression, ADHD, or high blood pressure because it keeps levels steady and improves adherence. But IR is better for acute symptoms-like sudden pain, panic attacks, or when you’re starting a new medication and need to adjust the dose quickly. The best choice depends on your condition, lifestyle, and how your body responds.
What happens if I accidentally crush an ER pill?
Crushing an extended-release pill releases the entire dose all at once, which can cause a toxic surge of medication in your bloodstream. For example, crushing an ER opioid can lead to respiratory failure or death. Crushing bupropion ER can trigger seizures. If this happens, call poison control immediately (1-800-222-1222) or go to the ER. Do not wait for symptoms to appear.
Can I switch from IR to ER or vice versa on my own?
Never switch between IR and ER formulations without your doctor’s guidance. The dosing isn’t always equal. For example, 30mg of Adderall IR is not the same as 30mg of Adderall XR. ER versions are often formulated with a different total dose to account for slow release. Switching on your own can lead to underdosing, overdosing, or dangerous side effects. Always consult your prescriber before changing your medication form.
Are ER medications more expensive? Is it worth it?
Yes, ER versions usually cost 15% to 25% more than IR. For example, Adderall XR can be $100 more per month than IR. But the higher cost often pays off. Better adherence means fewer missed doses, fewer doctor visits, and lower risk of hospitalization. A 2022 study found ER users had 22% higher adherence rates, which translates to fewer complications and long-term savings. If cost is an issue, ask about generic options or patient assistance programs.
Do ER medications work the same for everyone?
No. Factors like age, weight, liver function, and digestive health affect how ER drugs are absorbed. People with gastroparesis (slow stomach emptying) may absorb ER meds too quickly, leading to higher-than-expected drug levels. Older adults or those with kidney disease may process them slower. That’s why your doctor needs to monitor your response and adjust doses accordingly. What works for one person might be unsafe for another.


Sydney Lee
December 29, 2025 AT 11:26Let me just say, if you’re splitting ER pills to save money, you’re not being frugal-you’re playing Russian roulette with your neurochemistry. The fact that people think a scored line equals ‘safe to divide’ is terrifying. That’s not a coupon, it’s a pharmacokinetic landmine. And no, your ‘I’ve been doing it for years’ anecdote doesn’t override basic pharmacology. This isn’t a suggestion. It’s a warning written in blood.
oluwarotimi w alaka
December 30, 2025 AT 19:29u.s. pharma companies be like: ‘ohhh lets make pills that dont work right unless u swallow whole’… but in nigeria we just take the whole bottle when we feel bad. no fancy tech needed. why u guys make medicine so complicated? we dont even have pills that last 12hrs… we just drink more water and pray. maybe ur problem is not the pill… its ur brain.
Debra Cagwin
January 1, 2026 AT 14:22For anyone reading this and feeling overwhelmed-please know you’re not alone. Many of us have been there: confused, scared, tempted to take that extra pill because ‘it’s not doing anything yet.’ But you’re doing the right thing by seeking clarity. Talk to your pharmacist. Write down your questions. Bring a friend to your appointment. Small steps matter. Your body deserves patience, not panic. You’ve got this.
Hakim Bachiri
January 2, 2026 AT 19:03Look… I get it. You want to ‘optimize’ your meds. But crushing XR pills? That’s not biohacking-that’s just being a dumbass with a mortar and pestle. I’ve seen guys do it to get high. I’ve seen grandmas do it to ‘save cash.’ And I’ve seen ERs turn into emergency room visits. The FDA didn’t make these rules because they hate you. They made them because people like you keep dying. Stop. Just… stop.
Gran Badshah
January 4, 2026 AT 04:55bro i took my bupropion xl and split it because the bottle was running low… felt fine for 2 days… then my hands started shaking like i was in a quake. turned out i got a serotonin spike. now i just take the whole thing and eat a banana. works better anyway. dont be a hero.
Ellen-Cathryn Nash
January 5, 2026 AT 05:40It’s not just about the pills-it’s about the silence. The shame. The fear of asking, ‘Wait, does this thing take hours to work?’ We’re taught to ‘tough it out,’ to ‘be strong,’ to ‘not be a burden.’ But medication isn’t a moral test. It’s science. And science doesn’t care how brave you think you are. It only cares if you follow the damn instructions.
Samantha Hobbs
January 5, 2026 AT 06:31my mom took her ER antidepressant and thought it wasn't working so she took another one. then she passed out at the grocery store. now she's on IR and we all just use alarms. also she won't stop calling me at 3am to ask if she's 'still alive.' thanks, science.
sonam gupta
January 6, 2026 AT 02:53in india we dont have xr pills most of the time so we take ir 3x a day and call it a day. no one splits pills. we just remember. its called discipline. you americans make everything a medical mystery.
Julius Hader
January 6, 2026 AT 11:11Just wanted to say: I’ve been on XR sertraline for 5 years. Took me 6 weeks to feel anything. I almost quit. But I stuck with it. Now I’m stable. No crashes. No panic. Just… peace. Don’t give up. The slow burn is the real win. 🙏
Payton Daily
January 7, 2026 AT 02:45Think about it. Life is a slow drip. Not a splash. We want instant results-fast food, quick fixes, overnight success. But your brain? It’s not a video game. You don’t level up by spamming the button. The pill is just a tool. The real work is waiting. Sitting with the silence. Letting the medicine do its quiet job. That’s the real hero’s journey. Not the pill. The patience.