Antihistamine Safety Checker for Older Adults
This tool helps you determine if a medication contains high-risk sedating antihistamines that could increase fall risk for older adults. Enter a medication name or active ingredient to check its safety profile.
Every year, nearly one in four older adults falls. For many, the cause isn’t just slippery floors or poor lighting-it’s a medication they took for a runny nose or trouble sleeping. First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and brompheniramine are still widely used by older adults, often without knowing the risks. These drugs, sold over the counter as sleep aids or allergy relievers, can seriously impair balance, slow reaction time, and cause dizziness-making falls not just possible, but likely.
Why Sedating Antihistamines Are Dangerous for Older Adults
First-generation antihistamines cross the blood-brain barrier easily. That’s how they work-they block histamine in the brain to reduce allergy symptoms and induce drowsiness. But in older adults, this same effect becomes dangerous. Their bodies process these drugs slower. A healthy 30-year-old might clear diphenhydramine in about 8.5 hours. In someone over 65, that time stretches to over 13 hours. The sedation lasts longer, and the risk of falling rises with every passing hour.
Studies show these medications don’t just make you sleepy-they disrupt your balance system. One 2025 study tracking nearly 200,000 older adults found that 8% of those who filled a prescription for a first-generation antihistamine fell badly enough to need medical care within two months. That’s not a small number. It’s a pattern. The American Geriatric Society lists these drugs as potentially inappropriate for seniors in their Beers Criteria, a trusted guide for safe prescribing. Why? Because they don’t just cause drowsiness. They also cause confusion, dry mouth, blurred vision, constipation, and even delirium in hospitalized seniors.
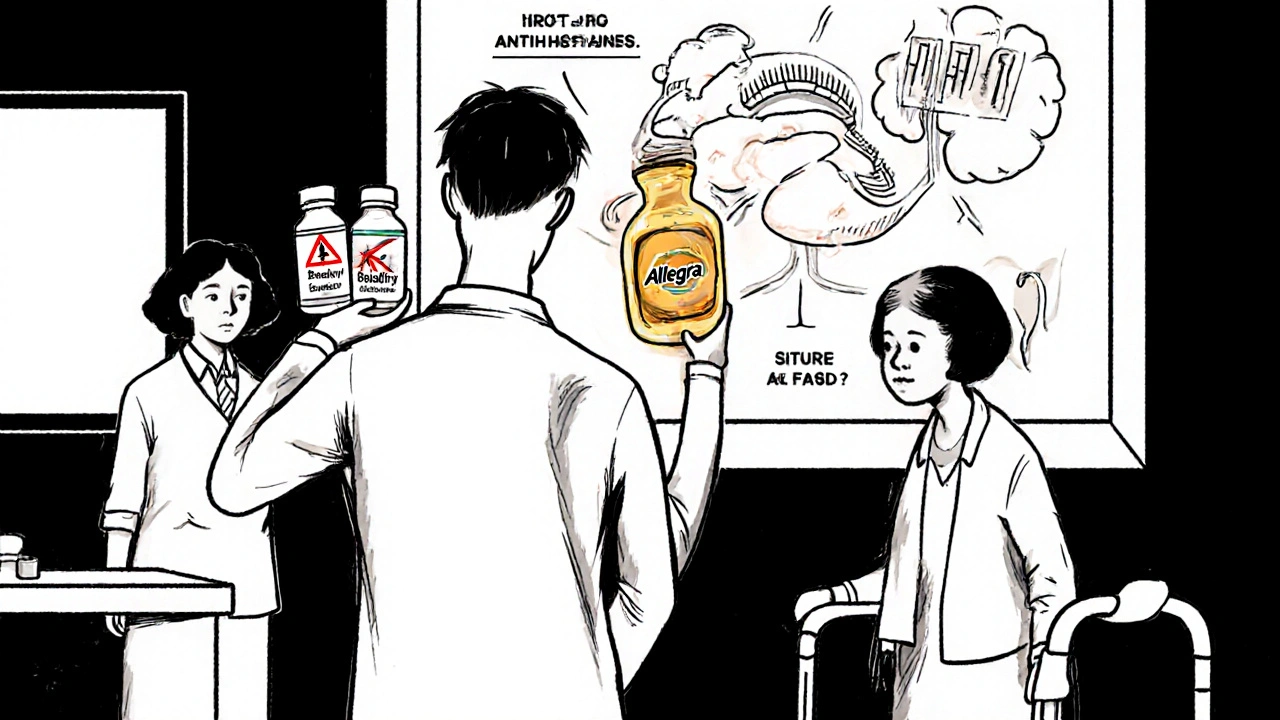
Compare that to second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra). These were designed to stay out of the brain. They don’t cross the blood-brain barrier the same way. As a result, they cause drowsiness in only 6-14% of users, compared to 15-20% for diphenhydramine. The difference isn’t subtle-it’s life-changing.
The Real Cost: Falls, Fractures, and Death
Falls aren’t just bruises and scrapes. In older adults, they lead to broken hips, head injuries, hospitalizations, and death. A 2018 meta-analysis published in Osteoporosis International found that seniors taking first-generation antihistamines had a 54% higher risk of an injurious fall and a 43% higher risk of fracture. The CDC reports over 36 million falls among older adults each year in the U.S. alone, with 32,000 resulting in death.
And here’s the kicker: many of these falls happen within hours of taking the medication. Peak sedation occurs 1-3 hours after ingestion and can linger for 6-8 hours. That’s why someone might take diphenhydramine at night to sleep-and then stumble in the bathroom at 3 a.m. Or take it in the morning for allergies and then fall while walking to the grocery store by noon.
What makes this worse is that doctors and pharmacists often don’t realize how common these drugs are. A 2019 study found that first-generation antihistamines were prescribed at nearly the same rate to older and younger patients-even though the risks are far higher for seniors. Over-the-counter labels don’t scream danger. They say “helps you sleep” or “relieves allergy symptoms.” They don’t say, “This could break your hip.”
Switching to Safer Alternatives
The good news? There are safer options. Second-generation antihistamines are just as effective for allergies but carry a fraction of the fall risk. Fexofenadine (Allegra) has the lowest sedation rate-only 6% in older adults. Loratadine (Claritin) is close behind. Cetirizine (Zyrtec) is slightly more sedating (14%) but still much safer than diphenhydramine.
Here’s a quick comparison:
| Medication | Generation | Anticholinergic Score | Drowsiness Rate in Seniors | Fall Risk Increase |
|---|---|---|---|---|
| Diphenhydramine (Benadryl) | First | 4 | 15-20% | Up to 87% |
| Chlorpheniramine (Chlor-Trimeton) | First | 3 | 12-18% | 72% |
| Cetirizine (Zyrtec) | Second | 1 | 14% | Not significant |
| Loratadine (Claritin) | Second | 0 | 6% | Not significant |
| Fexofenadine (Allegra) | Second | 0 | 6% | Not significant |
The Anticholinergic Cognitive Burden Scale rates drugs from 0 to 3-4. A score of 3-4 means strong anticholinergic effects-linked to memory loss, confusion, and falls. First-generation antihistamines score 3-4. Second-generation score 0-1. That’s not a minor difference. It’s the difference between staying independent and ending up in a hospital.
Non-Medication Ways to Manage Allergies and Sleep
Do you really need a pill for every sneeze or night of poor sleep? Often, the answer is no.
For allergies:
- Use saline nasal rinses-studies show they reduce symptoms by 35-40%
- Switch to allergen-proof bedding-they cut dust mite exposure by 83%
- Install a HEPA air filter-they remove 99.97% of airborne allergens
For sleep:
- Stick to a regular bedtime and wake time-even on weekends
- Avoid caffeine after noon
- Keep your bedroom cool, dark, and quiet
- Get sunlight in the morning to reset your body clock
These aren’t just “nice-to-haves.” They’re proven, safe, and free-or low-cost. And they don’t make you dizzy.
What You Can Do Right Now
If you or someone you care for is over 65 and taking diphenhydramine, chlorpheniramine, or any other first-generation antihistamine, here’s what to do:
- Check every medication-including OTC pills, sleep aids, and cold remedies. Many contain hidden antihistamines.
- Ask your doctor or pharmacist: “Is this medication safe for someone my age? Are there safer alternatives?”
- Switch to fexofenadine or loratadine if you need an antihistamine. They work just as well without the dizziness.
- Don’t stop cold turkey-if you’ve been taking it for sleep, work with your provider to replace it with sleep hygiene habits first.
- Do a “brown bag review”-take all your medications (including vitamins and supplements) to your pharmacist for a free review. They’ll find hidden risks you might miss.
Pharmacist-led reviews have been shown to reduce fall risk by 26%. That’s a huge win.

Make Your Home Safer Too
Even if you switch medications, fall risk doesn’t disappear overnight. Combine medication changes with home safety:
- Install grab bars in the bathroom
- Add bright, motion-sensor lights in hallways and bathrooms
- Remove loose rugs and clutter from walkways
- Use non-slip mats in the shower
- Keep a phone or emergency button within reach
These changes can reduce fall risk by up to 32%. When paired with safer meds, the results are even better.
The Bigger Picture: Why This Keeps Happening
Despite decades of evidence, first-generation antihistamines are still among the top three OTC sleep aids sold to seniors. In 2024, over 28 million units of diphenhydramine were sold to people aged 65 and older in the U.S. That’s $142 million in sales-despite clear warnings.
Why? Because they’re cheap, easy to buy, and widely promoted. The FDA added stronger warnings to labels in 2020, but they’re buried in small print. Most people don’t read them. And many doctors still prescribe them out of habit.
But things are changing. The CDC updated its STEADI toolkit in January 2025 to include a new medication risk module. Medicare now requires fall risk assessments that include a review of all sedating medications-including antihistamines. And two new antihistamines designed specifically for older adults are in clinical trials, with early results showing 89% less drowsiness than diphenhydramine.
This isn’t just about one drug. It’s about how we treat older adults in medicine. We need to stop assuming that what works for a 40-year-old works for a 75-year-old. Our bodies change. Our risks change. Our meds should too.
Are all antihistamines dangerous for older adults?
No. Only first-generation antihistamines like diphenhydramine and chlorpheniramine carry high fall risk. Second-generation options like fexofenadine (Allegra), loratadine (Claritin), and cetirizine (Zyrtec) are much safer. They’re just as effective for allergies and cause far less drowsiness and dizziness.
Can I just take a lower dose of diphenhydramine to stay safe?
Lowering the dose reduces risk slightly, but it doesn’t eliminate it. Even 12.5 mg of diphenhydramine can cause dizziness and balance problems in older adults. The body processes it slower, so effects last longer. Safer alternatives exist-switching is better than cutting the dose.
I’ve been taking Benadryl for sleep for years. How do I stop?
Don’t stop suddenly. Work with your doctor to replace it with non-drug sleep strategies: fixed bedtime, no screens before bed, cool dark room, and morning sunlight. You may have trouble sleeping at first-but that’s temporary. Most people adjust within 1-2 weeks. The benefits-better balance, less confusion, fewer falls-are worth it.
My doctor prescribed this. Should I still question it?
Yes. Doctors are human. They may not know the latest guidelines or may have been taught to use these drugs decades ago. The American Geriatric Society’s Beers Criteria is clear: avoid first-generation antihistamines in older adults. Ask your doctor: “Is there a safer option?” If they hesitate, ask for a pharmacist consultation.
What should I look for on the label to avoid these drugs?
Look for these active ingredients: diphenhydramine, chlorpheniramine, brompheniramine, doxylamine, or pyrilamine. These are all first-generation antihistamines. Avoid products labeled “PM,” “nighttime,” or “for sleep” unless you’ve confirmed the ingredients. Even allergy meds can contain them.
Next Steps: Protect Yourself or a Loved One
Start today. Take a look at every bottle in the medicine cabinet. Write down every medication, including vitamins and OTC pills. Bring that list to your next doctor or pharmacist visit. Ask: “Which of these could make me or my loved one fall?”
It’s not about fear. It’s about control. You don’t have to live with dizziness or fear of falling. Safer choices exist. Simple changes work. And with the right steps, you can protect independence, health, and life itself.


Jamie Watts
November 16, 2025 AT 18:14Why are we even talking about this like it’s a new discovery? I’ve been telling my grandma for years not to take Benadryl for sleep and she still does it because it’s ‘natural’ and ‘cheap’-like that matters when you’re lying in the ER with a broken hip. The data’s right there in black and white. People just don’t want to change.
Latrisha M.
November 17, 2025 AT 07:44This is exactly why we need better education for seniors and their families. I work in home health and see this every week. Grandparents taking OTC meds because they think it’s harmless. No one tells them the risks. Pharmacists are the unsung heroes here-free med reviews should be standard, not optional.
Teresa Smith
November 17, 2025 AT 18:54It’s not just about the drugs. It’s about a culture that treats aging as a problem to be medicated rather than a phase of life to be supported. We’ve normalized sedation as a solution for sleep and allergies. We’ve forgotten that the body changes. We’ve stopped listening to older adults’ lived experience. This isn’t medical advice-it’s a call to rethink how we value elder care.
Danish dan iwan Adventure
November 19, 2025 AT 11:47Anticholinergic burden >3 is a CNS toxin in geriatric populations. First-gen H1 blockers are pharmacologically obsolete for seniors. Second-gen agents exhibit negligible BBB penetration. Clinical guidelines are unequivocal. Non-pharmacological interventions are first-line. End of discussion.
Rachel Wusowicz
November 20, 2025 AT 08:58Have you noticed how every single ‘sleep aid’ and ‘allergy relief’ product is designed to make you drowsy? It’s not an accident. Big Pharma knows if you’re sleepy, you’re less likely to question your meds. They’ve been pushing these drugs for decades-because profit > safety. The FDA warnings? Buried under 10-point font. They want you confused, dizzy, and dependent. This isn’t medicine-it’s manipulation.
ZAK SCHADER
November 22, 2025 AT 00:18I dont know why people make such a big deal about this. I take diphenhydramine every night and I’m 72. Never fallen. Maybe its just me. Also why are we switching to fancy brand names like Allegra? Benadryl works fine. If you dont like it dont take it. Stop telling old people what to do.
Ankit Right-hand for this but 2 qty HK 21
November 22, 2025 AT 06:33Are you serious? You’re telling me to stop taking Benadryl because some study says I might fall? What about the 90% of seniors who take it and don’t fall? This is fearmongering wrapped in data. You want to take away our only sleep aid and replace it with ‘sleep hygiene’? That’s a joke. I don’t have time to ‘stick to a bedtime’-I work two jobs. This is elite nonsense.
Diane Tomaszewski
November 23, 2025 AT 07:24I used to take Benadryl for allergies and felt like I was walking through molasses. When I switched to Claritin, it was like waking up. I didn’t even realize how bad it was until it was gone. Simple swap. Big difference. Why aren’t we all doing this?
Melanie Taylor
November 24, 2025 AT 16:23My mom switched to Zyrtec last year and her balance improved so much she started gardening again 🌿 She said she felt like herself for the first time in years. Please, if you’re over 65 and taking anything with ‘PM’ or ‘nighttime’ in the name-check the label. It could change your life.
Oyejobi Olufemi
November 26, 2025 AT 07:18Who authorized this? Who gave you the right to decide what older people should take? This is medical authoritarianism. The government, the FDA, the geriatric society-they’re all part of the same system that wants to control our bodies under the guise of ‘safety.’ You think you’re helping? You’re eroding autonomy. Let people choose. Let them risk. That’s freedom. You don’t get to sanitize aging. You don’t get to make us safe. We are not children.