Fibromyalgia isn’t just feeling tired or sore. It’s a constant, deep ache that moves around your body - sometimes in your shoulders, then your hips, then your knees - with no clear trigger. You might wake up exhausted even after eight hours of sleep, struggle to remember simple words, or feel overwhelmed by loud noises or bright lights. For millions, this isn’t occasional discomfort. It’s life. And it’s real.
What Fibromyalgia Actually Is
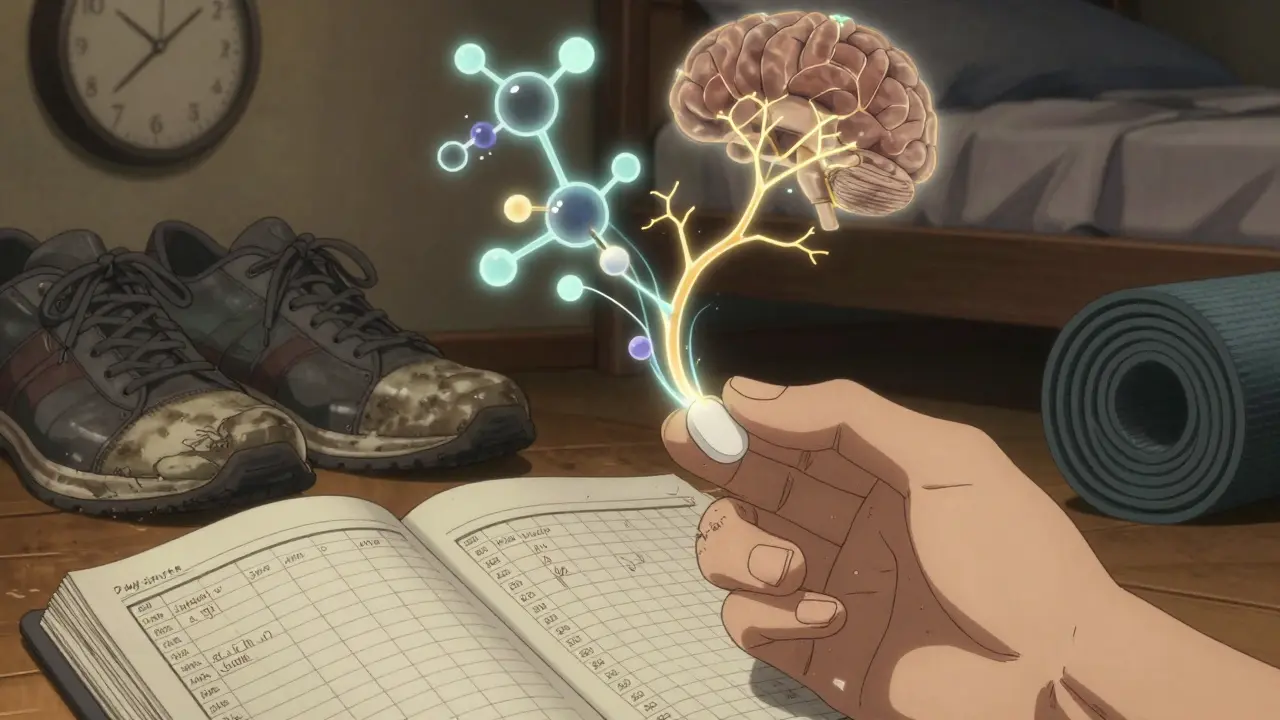
Fibromyalgia is a neurological condition where the brain and spinal cord process pain signals differently. It’s not arthritis. It’s not muscle damage. It’s your nervous system turned up too loud. The American College of Rheumatology defines it by two main things: widespread pain lasting at least three months and at least four other symptoms like fatigue, trouble sleeping, memory issues (called ‘fibro fog’), or feeling emotionally drained.
It’s not rare. Around 2 to 8% of people worldwide have it. In the U.S., that’s about 10 million people. And women make up 75 to 90% of diagnoses. Why? No one knows for sure. Hormones, genetics, trauma, or how the body handles stress may all play a role. But the key thing to understand: fibromyalgia isn’t ‘in your head.’ It’s in your nerves.
Why Antidepressants Are Used - Even If You’re Not Depressed
Here’s where things get confusing. You’re prescribed an antidepressant, but you don’t feel sad. You don’t cry all day. So why take it?
Antidepressants like duloxetine, milnacipran, and amitriptyline don’t work here because they fix mood. They work because they change how pain signals travel through your nervous system. These drugs increase levels of serotonin and norepinephrine - chemicals that help calm down overactive pain pathways. It’s like turning down the volume on a speaker that’s blasting 24/7.
Three antidepressants are FDA-approved specifically for fibromyalgia:
- Duloxetine (Cymbalta): An SNRI. Starts at 30 mg daily, often increased to 60 mg. Works in 4 to 6 weeks. Helps with pain and fatigue.
- Milnacipran (Savella): Another SNRI. Begins at 12.5 mg, builds up to 100 mg daily. Similar timeline, similar results.
- Amitriptyline: A tricyclic antidepressant. Not FDA-approved for fibromyalgia, but widely used. Starts at just 5-10 mg at bedtime. Helps with sleep and pain. Many patients report their first good night’s sleep in years.
Studies show these medications reduce pain by 20-30% in people who respond. But here’s the catch: only about half of patients see real benefit. And side effects? They’re common. Dry mouth, dizziness, weight gain, nausea, and drowsiness can be so bad that 20-30% of people stop taking them.
The Real Star of Treatment: Exercise
There’s one treatment that consistently outperforms all medications: movement.
Exercise isn’t just ‘good for you’ - it’s the most powerful tool we have. A 2023 review from the American College of Rheumatology found that regular, gentle activity reduces pain by 25-35% in 70% of patients after six months. That’s better than any pill.
But it’s not about running marathons. It’s about starting small. Try 10-15 minutes of walking, tai chi, or yoga two or three times a week. Gradually add five minutes every week. The rule? Never push through pain. If you feel worse the next day, you went too far. Back off. Slow and steady wins.
Tai chi, in particular, has shown up in studies as a game-changer. One trial found a 20-30% drop in pain after just 12 weeks. Yoga? A 2022 Arthritis Foundation study showed a 24% reduction in pain intensity. And Pilates? Helps with stiffness and balance - two big problems for people with fibromyalgia.
Why does it work? Movement helps your body relearn how to handle pain. It reduces inflammation, improves sleep, and boosts natural painkillers like endorphins. It also gives you back control - something fibromyalgia takes away.
What About Other Treatments?
Medication isn’t the whole story. The best results come from combining approaches.
Cognitive Behavioral Therapy (CBT) helps retrain how you think about pain. Eight to twelve weekly sessions can reduce pain and improve daily function by 20-30%. It doesn’t erase pain, but it helps you live with it better.
Acupuncture is another option. NHS data shows about 60% of people get 15-25% pain relief after 6-12 sessions. It’s not magic, but it’s low-risk and worth trying if other things haven’t worked.
And then there’s pregabalin (Lyrica). It’s not an antidepressant - it’s a nerve-calming drug. It helps 25-40% of patients, but side effects are heavy: dizziness in 30-40%, sleepiness in 20-30%, and weight gain in 10-15%. Many patients rate it as ‘moderately helpful’ but ‘very hard to tolerate.’
Some people find relief with heat therapy, massage, or mindfulness. Others swear by the Quell device - a wearable nerve stimulator cleared by the FDA. It’s not cheap, but for some, it’s life-changing.
How Treatment Actually Works - Step by Step
There’s no quick fix. Treatment is a process.
Weeks 1-4: You’re learning. Your doctor explains fibromyalgia. You start tracking symptoms. You begin gentle movement - even just walking around the block. Sleep hygiene matters: no screens before bed, same bedtime every night.
Weeks 4-8: If you’re starting medication, this is when you begin. Amitriptyline might start at 5 mg at night. Duloxetine at 30 mg. You watch for side effects. You keep moving. You might join a CBT program.
Weeks 8-12: This is when things start to shift. Sleep improves with amitriptyline. Pain begins to ease with SNRIs. Exercise starts to feel less like a chore and more like a tool. You notice you can get through the day without collapsing.
Months 3-6: You’re building a routine. You’ve found the right mix: maybe 30 minutes of yoga three times a week, 10 mg of amitriptyline at night, and daily breathing exercises. You’re not cured. But you’re managing.
Many people fail because they expect pills to fix everything. The truth? Medication helps, but it’s a support system - not the foundation.

What Doesn’t Work - And Why
There’s a lot of noise out there. Opioids? The CDC says don’t use them for fibromyalgia. They don’t help long-term and carry serious risks. Steroids? Useless. Anti-inflammatories? Usually no effect - fibromyalgia isn’t an inflammatory disease.
And here’s the hard truth: many doctors still don’t get it. Patients wait an average of five years to get diagnosed. Some are told it’s ‘all in their head.’ That’s changing - slowly - thanks to research showing fibromyalgia is a real neurological condition, not a mental health issue.
Still, access to care is uneven. In cities, you might find a pain specialist who knows about CBT and graded exercise. In rural areas? You’re lucky if you get a referral. Insurance often won’t cover non-drug treatments. Only 35% of plans cover CBT for fibromyalgia, according to a 2023 KFF analysis.
Real Stories, Real Results
One woman on MyFibroTeam wrote: ‘I’d been on 10 different meds. Nothing worked. Then I started 10 mg of amitriptyline at night. After two weeks, I slept through the night for the first time in 10 years. I didn’t feel ‘cured,’ but I felt like I could breathe again.’
Another said: ‘I tried duloxetine at 60 mg. It made me feel like I was having panic attacks every day. I went back to 20 mg. Still helped with pain. Still caused nausea. But I added tai chi three times a week. Now I can walk my dog without crying.’
On Reddit’s fibromyalgia community, 68% said exercise was the most helpful thing they’d ever done. Only 42% said antidepressants helped - and half of them said the side effects almost made them quit.
What’s Next?
Research is moving fast. The NIH just funded $15 million to study how fibromyalgia affects the brain. A new drug called centanafadine showed 35% pain reduction in trials - better than current options, with fewer side effects. It’s under FDA review.
Future treatments may be personalized. Are you pain-dominant? Fatigue-dominant? Sleep-dominant? Your treatment could be tailored to your specific pattern.
But for now, the best advice hasn’t changed: move gently, sleep well, manage stress, and use medication wisely - not as a crutch, but as one tool in a bigger toolkit.
You’re not broken. Your body is just wired differently. And with the right approach, you can live well - even with chronic pain.
Can antidepressants cure fibromyalgia?
No. Antidepressants don’t cure fibromyalgia. They help manage symptoms like pain, fatigue, and sleep problems by changing how your nervous system processes signals. They’re one part of a larger plan - not a solution on their own.
Why do doctors prescribe antidepressants if I’m not depressed?
They’re not prescribing them to treat depression. They’re using them because these drugs affect brain chemicals - serotonin and norepinephrine - that also control pain signals. Even if you feel fine emotionally, your nervous system may be overreacting to pain. These medications help calm that reaction.
How long does it take for antidepressants to work for fibromyalgia?
It varies. Tricyclics like amitriptyline often improve sleep in 2-4 weeks. SNRIs like duloxetine usually take 4-6 weeks to reduce pain. Full benefits may take up to 12 weeks. Patience is key - and so is sticking with it, even if side effects show up early.
Is exercise really more effective than medication?
Yes, for long-term results. Studies show exercise reduces pain by 25-35% in 70% of people after six months. Medications help about half of users, but often with side effects that lead to stopping. Exercise builds resilience, improves sleep, and reduces flare-ups - and the benefits last even after you stop.
What’s the safest starting dose for amitriptyline in fibromyalgia?
Most doctors start at 5-10 mg at bedtime. This low dose helps with sleep and pain with minimal side effects. The dose is slowly increased - usually by 5 mg every week - until you find the right balance. Going too fast can cause drowsiness, dry mouth, or dizziness.
Can I stop taking antidepressants if I start exercising?
Don’t stop suddenly. Even if exercise is helping, talk to your doctor before making changes. Some people reduce their dose over time as their activity level increases. Others stay on a low dose long-term because it helps with sleep or pain. It’s a personal decision based on your symptoms and response.
What should I do if my doctor won’t prescribe an antidepressant?
Ask for a referral to a pain specialist or rheumatologist. Many primary care doctors aren’t trained in fibromyalgia management. You can also start with non-drug treatments right away: graded exercise, CBT, or sleep hygiene. These are proven to help - and they don’t require a prescription.


rahulkumar maurya
February 4, 2026 AT 04:08Let’s be real - most of these so-called ‘fibromyalgia experts’ haven’t even touched a patient in person. They just regurgitate NIH pamphlets while ignoring the real issue: systemic inflammation from glyphosate-laden food and EMF overload. You think antidepressants help? Try a 30-day keto reset + grounding mats. I’ve seen patients go from wheelchairs to marathons. The medical-industrial complex doesn’t want you to know this.
Demetria Morris
February 5, 2026 AT 09:24I’ve been on amitriptyline for 18 months. 10mg at night. Sleep improved. Pain? Still there. But I stopped expecting miracles. Exercise? I walk 10 minutes every other day. That’s it. No yoga. No tai chi. Just… movement. And honestly? That’s more than most people with this condition do. I’m not proud. I’m just surviving.
Geri Rogers
February 6, 2026 AT 08:15Y’all need to stop treating this like a puzzle you can solve with one magic pill 💪
Exercise isn’t ‘optional’ - it’s your new medication. I started with 5 minutes of stretching on my couch. Then 10. Then I walked to the mailbox. Now I do yoga with my dog. No fancy gear. No Instagram posts. Just me, my pain, and a mat.
And yeah, amitriptyline helped me sleep - but only because I stopped drinking coffee after 2pm. And turned off my phone at 9. And didn’t scroll doomthreads before bed.
You don’t need a PhD to manage this. You need consistency. And patience. And maybe a little self-compassion 🫂
P.S. If your doctor won’t prescribe low-dose amitriptyline? Find a new doctor. Your pain is real. You deserve better.
Samuel Bradway
February 8, 2026 AT 03:59I used to think meds were the answer. Then I realized I was just trying to numb the noise. Walking in the park for 15 minutes - no music, no podcast - that’s when I started feeling like myself again. Not cured. Just… less broken. The antidepressants? They helped me sleep. But the quiet walks? They helped me remember I still existed.
Caleb Sutton
February 8, 2026 AT 20:50Alex LaVey
February 9, 2026 AT 23:38Hey - if you’re reading this and you’re tired of being told it’s ‘all in your head,’ I see you.
It’s okay if you can’t do 30 minutes of yoga. It’s okay if you cry when the laundry pile looks too big. It’s okay if you miss work because your legs feel like concrete.
You’re not lazy. You’re not broken. You’re just navigating a body that speaks a language no one else learned.
Start small. One deep breath. One step. One glass of water. That’s enough today.
You’re doing better than you think.
Coy Huffman
February 11, 2026 AT 19:59amitriptyline 5mg at night changed my life. not because it killed the pain - but because i finally slept. like, real sleep. not just lying there with my brain screaming. i used to think meds were for weak people. then i realized: surviving is not weakness. it’s strategy.
also - tai chi is weird as hell but it works. like, ‘why am i moving like a drunk crane’ weird. but my hips stopped screaming. so i keep doing it.
and no, i don’t care if you think it’s placebo. if it lets me hold my kid without crying, i’m not arguing.
Amit Jain
February 13, 2026 AT 02:53My friend has fibro. She walks 10 min every day. That’s it. No pills. No yoga. Just walk. After 3 months, she said she could hold her coffee without shaking. That’s real. You don’t need fancy stuff. Just move a little. Every day. Even if you hate it.
Keith Harris
February 13, 2026 AT 05:05Let’s be honest - antidepressants for fibro is just pharma’s way of monetizing suffering. You’re not depressed. You’re furious. You’re exhausted. You’re angry no one believes you. But instead of fixing the system, they hand you a pill and tell you to ‘adjust your mindset.’
Meanwhile, the real culprits - environmental toxins, chronic stress, food deserts - are ignored. And guess who pays? The poor. The women. The ones who can’t afford CBT or a personal trainer.
This isn’t medicine. It’s capitalism with a stethoscope.
Kunal Kaushik
February 14, 2026 AT 11:51My mom has fibro. She does tai chi with a YouTube video every morning. No fancy studio. Just her, a mat, and her cat judging her. She says it’s not about pain anymore - it’s about feeling like she’s still in charge of something. That’s the real win.
Also - amitriptyline 10mg. She calls it her ‘sleep fairy dust.’ 😴💤
Jamillah Rodriguez
February 16, 2026 AT 06:25I tried everything. Medications? Made me vomit and gain 30 lbs.
Exercise? Made me cry on the treadmill.
CBT? The therapist asked me if I ‘felt heard.’ I screamed into a pillow.
Now I just stare at the ceiling and wait for the pain to get bored and leave.
It’s not a journey. It’s a prison with a wellness blog.
Susheel Sharma
February 16, 2026 AT 17:48The data is statistically significant but clinically negligible. Antidepressants reduce pain by 20-30% - a marginal effect size (Cohen’s d = 0.35). Exercise shows similar results, but with higher attrition rates due to poor adherence. The real issue? Publication bias. Positive outcomes are overrepresented. Negative trials are buried. The NIH’s $15M funding? Likely to yield another placebo-controlled trial with inadequate power. We need neuroimaging biomarkers - not more SSRIs.