More than 1 in 5 people worldwide have a fungal skin infection at any given time. It’s not rare. It’s not unusual. And yet, most people don’t know how to tell the difference between a simple rash and something that needs real treatment. You might think it’s eczema. Or maybe you assume it’s just sweat. But if your skin is red, itchy, peeling, or has a ring-shaped border, it could be something more - and it needs the right kind of care.
What’s Actually Growing on Your Skin?
Fungal skin infections come in two main flavors: ringworm and Candida. Don’t let the names fool you. Ringworm isn’t caused by worms. It’s caused by fungi called dermatophytes - mostly Trichophyton species. These fungi eat keratin, the protein in your skin, hair, and nails. That’s why they love the scalp, feet, groin, and nails. Candida, on the other hand, is yeast. It’s the same kind of fungus that causes thrush or vaginal yeast infections. But it can also live on your skin, especially in warm, damp places like under your breasts, in your armpits, or between your toes.
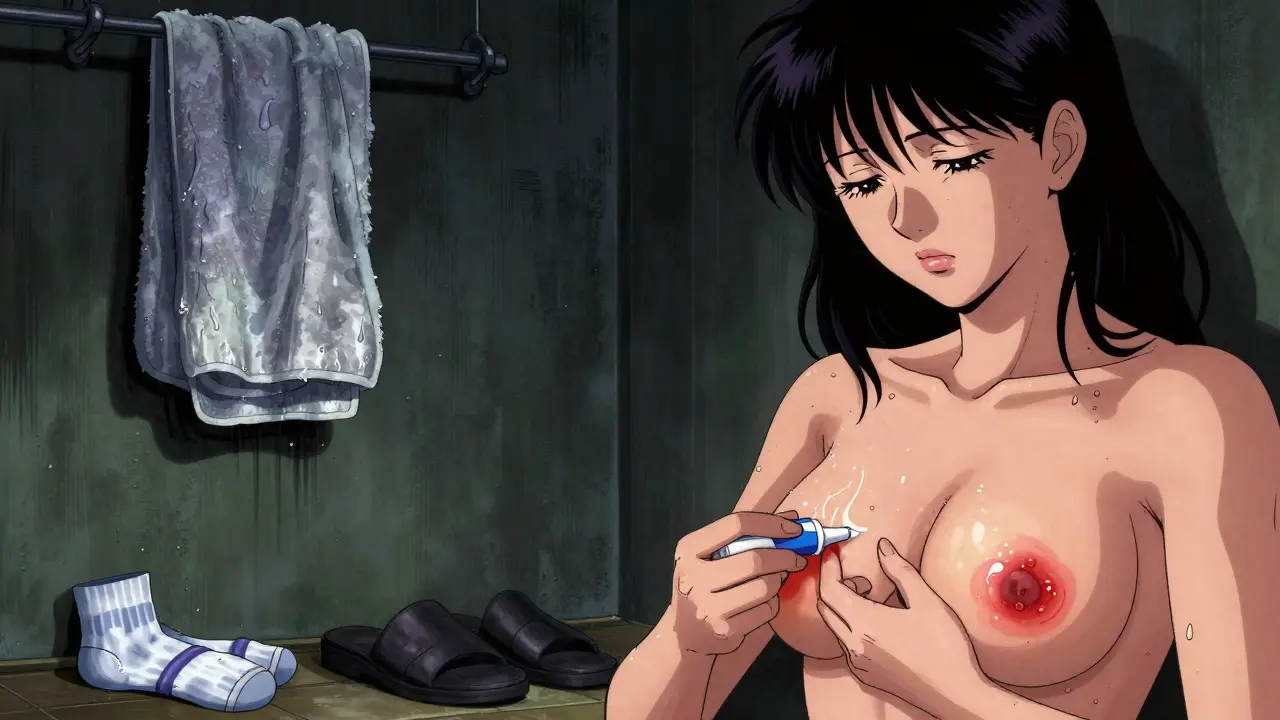
Ringworm shows up as a red, circular patch with a raised, scaly edge. The center often looks clearer, like a ring - hence the name. It can appear anywhere on the body. In kids, it’s common on the scalp. In adults, it’s often on the feet (athlete’s foot) or groin (jock itch). Candida infections look different. They’re not ring-shaped. Instead, they’re bright red, moist, and sometimes have tiny pimple-like bumps around the edges. They don’t flake like ringworm. They feel soggy.
How Do You Get These Infections?
You don’t need to be dirty to get a fungal infection. In fact, many people pick them up from perfectly clean surfaces. Ringworm spreads easily through direct contact - like shaking hands with someone who has it, or petting a dog or cat with a patchy coat. Kids are especially prone because they play on the floor, share towels, or use the same locker room. In adults, athlete’s foot is often caught from walking barefoot in gyms, pools, or communal showers.
Candida thrives where moisture builds up. Tight clothing, sweating a lot, or not drying off well after a shower can create the perfect environment. People with diabetes are more likely to get Candida because high blood sugar feeds the yeast. If you’re on long-term antibiotics or have a weakened immune system, your body’s natural defenses are down, and Candida can take over.
And here’s something many don’t realize: fungal infections can come back. About 1 in 3 people who’ve had ringworm or Candida on their skin get it again within a year. Why? Because the fungus doesn’t always die completely. It hides in skin folds, under nails, or even in your shoes.
How Doctors Diagnose It
Most doctors can guess what it is just by looking. But guessing isn’t always right. A 2022 study found that primary care doctors correctly identify ringworm only about half the time. Dermatologists get it right 85% of the time. That’s why so many people end up using steroid creams - thinking it’s eczema - and make things worse.
The best way to be sure? A simple test. A doctor scrapes a bit of skin or nail and puts it under a microscope after treating it with potassium hydroxide (KOH). If you see fungal threads, it’s confirmed. Culture tests take longer - two to four weeks - but they can tell you exactly which fungus you have. Newer tests using DNA analysis are faster and more accurate, but not yet available everywhere.
Don’t wait for a test if the signs are classic. If you have a clear ring-shaped rash with scaling, it’s almost certainly ringworm. If you have a red, moist patch with little pustules around the edge, especially in a skin fold, it’s likely Candida. Treating early stops it from spreading.
Topical Antifungals: What Works and What Doesn’t
For most cases, you don’t need pills. Creams, sprays, and powders work just fine - if you use them right.
For ringworm, terbinafine (Lamisil) is the gold standard. It kills the fungus faster than other creams. Apply it once or twice a day for at least two weeks, even if the rash looks gone after five days. Stopping early is why it comes back. Clotrimazole (Lotrimin) is another common option. It’s a bit slower but still effective. Both are available over the counter.
For Candida, clotrimazole and miconazole are top choices. They work well on skin folds and diaper rashes. Nystatin is often used for babies. Apply it after cleaning and drying the area. Keep the skin as dry as possible. Use talc-free powders to absorb moisture.
Don’t use steroid creams like hydrocortisone unless your doctor says so. They calm redness and itching, but they don’t kill fungus. In fact, they can make the infection spread deeper and harder to treat.
When You Need Oral Medication
Topical treatments fail when the fungus is deep - like under your nails or in thick skin. That’s where oral meds come in.
For nail infections (tinea unguium), terbinafine is still the go-to. You take it daily for 6 to 12 weeks. It works because it builds up in the nail and kills the fungus as the nail grows out. But it’s not harmless. About 1 in 100 people get liver enzyme changes. Your doctor should check your liver before and during treatment.
For widespread or stubborn Candida, fluconazole is often prescribed. One pill a week for a few weeks usually clears it up. But here’s the catch: resistance is rising. Some strains of Candida, especially in hospitals, no longer respond to fluconazole. That’s why new drugs like ibrexafungerp (Brexafemme) were approved in 2023 - for recurrent vaginal yeast infections that won’t respond to older drugs.
There’s also a new problem: terbinafine resistance. Around 5-7% of Trichophyton rubrum strains in North America are now less sensitive to it. That means some people who take terbinafine don’t get better. Doctors are starting to switch to itraconazole or griseofulvin in those cases.
What People Are Doing at Home
Reddit and Healthgrades are full of stories. One user in Manchester said she had ringworm on her arm for months. She tried everything - tea tree oil, coconut oil, vinegar rinses. Nothing worked. Then she bought Lamisil cream. Two weeks later, the ring was gone. Another person said his Candida diaper rash cleared up after switching from cloth diapers to breathable disposables and using clotrimazole twice a day.
Some people swear by probiotics. A 2023 Instagram poll of 850 people with recurrent yeast infections found that 65% had fewer flare-ups when they took Lactobacillus supplements alongside antifungals. It’s not a cure, but it might help your body rebalance.
But don’t rely on home remedies alone. Apple cider vinegar, garlic, or essential oils have no strong scientific backing. They might soothe, but they won’t kill the fungus. If it’s not better in two weeks, see a doctor.

Prevention: The Real Secret
The best treatment is avoiding the infection in the first place.
- Always dry your skin thoroughly after showering - especially between toes, under breasts, and in the groin.
- Wear flip-flops in public showers and locker rooms.
- Don’t share towels, shoes, or hairbrushes.
- Change out of sweaty clothes right after working out.
- If you have pets with patchy fur, get them checked - they could be the source.
- For babies, change diapers frequently and let skin air out when possible.
- Keep blood sugar under control if you have diabetes.
And here’s a tip most people miss: wash your socks and underwear in hot water. Fungi survive in fabric. Cold washes won’t kill them.
The Bigger Picture
Fungal infections aren’t just annoying - they’re growing more dangerous. The CDC now tracks Candida auris, a drug-resistant yeast that sticks to skin and spreads in hospitals. It’s been found in 27 U.S. states. It doesn’t always cause symptoms, but it can be deadly in people with weak immune systems.
Meanwhile, the global antifungal market hit $14.7 billion in 2022. That’s how big this problem is. And with climate change making warm, humid conditions more common, fungal infections could become even more widespread.
But there’s hope. New drugs are being developed. Research into the skin’s microbiome - the balance of good and bad microbes - is opening new doors. Scientists are now looking at how to boost good bacteria to keep fungi in check, instead of just killing them.
The message? Don’t ignore a weird rash. Don’t guess. Don’t use steroid cream on a ring-shaped patch. See a doctor if it doesn’t improve in two weeks. And if you’ve had it before, take prevention seriously. Fungal infections are common. But they don’t have to be a recurring nightmare.
Can fungal skin infections spread to other people?
Yes, especially ringworm. It spreads through direct skin contact, sharing towels, or touching infected pets. Candida is less contagious but can spread in warm, moist environments like shared showers or through poor hygiene. Always avoid sharing personal items and wash your hands after touching infected skin.
How long does it take for antifungal cream to work?
You’ll usually see improvement in 3-7 days, but you need to keep using the cream for the full course - often 2-4 weeks for ringworm and 1-2 weeks for Candida. Stopping early is the #1 reason infections come back.
Is it safe to use antifungal cream on my child?
Yes, most over-the-counter antifungals like clotrimazole and miconazole are safe for children. For diaper rash, nystatin is often recommended. Always check the label for age recommendations and avoid using steroid creams unless directed by a doctor.
Can I get fungal infections from my pets?
Absolutely. Cats and dogs, especially those with patchy hair or flaky skin, can carry ringworm fungi. If your pet has a rash or is losing hair, take them to the vet. Wash your hands after petting them, and don’t let them sleep on your bed if they’re infected.
Why does my fungal infection keep coming back?
Fungi hide. They live in your shoes, under your nails, in your towels, or in skin folds you didn’t fully dry. If you don’t treat the whole area or clean your environment, the fungus returns. Use antifungal powder in shoes, wash clothes in hot water, and keep skin dry. Recurrence is common - but preventable.
Are there natural remedies that work?
Tea tree oil, coconut oil, and apple cider vinegar may help soothe symptoms, but there’s no strong evidence they kill the fungus like prescription or OTC antifungals do. Don’t rely on them alone. Use them as a supplement to proven treatments, not a replacement.
Should I take probiotics for fungal skin infections?
Some people find that taking Lactobacillus probiotics helps reduce recurrent Candida infections, especially in the groin or vaginal area. While not a cure, it may help restore your body’s natural balance. Talk to your doctor before starting supplements, especially if you’re immunocompromised.
What to Do Next
If you have a rash that’s not improving, start with an OTC antifungal cream. Apply it twice daily for at least two weeks. If it doesn’t clear up, or if it spreads, see a doctor. Don’t wait. The longer you wait, the harder it becomes to treat - and the more likely you are to pass it on.
And if you’ve had one before, make prevention part of your routine. Dry well. Wash your socks. Keep your skin clean and dry. Fungal infections are common, but they’re not inevitable.


Indra Triawan
January 5, 2026 AT 22:27So many people think it's just a rash... but honestly, if your skin feels like it's breathing fungus, you know it's not normal. I had this ringworm on my elbow for months, thought it was dry skin. Turns out, I was just feeding it with lotion. 😅
Lily Lilyy
January 6, 2026 AT 19:11You are so right to raise awareness about this! 🌟 So many people suffer in silence, thinking it's embarrassing. But fungal infections are just as normal as catching a cold. You deserve to feel better - and you can! 💪❤️
Joann Absi
January 8, 2026 AT 14:46OMG I CAN'T BELIEVE PEOPLE STILL USE TEA TREE OIL LIKE IT'S A CURE 🤡 I mean, come on - we have science now! 🧪 My cousin used coconut oil for 6 months and ended up with a fungal tattoo on her thigh. 🤮
Mukesh Pareek
January 8, 2026 AT 22:56The clinical misdiagnosis rate is statistically significant - 50% in primary care versus 85% in dermatology. This reflects a systemic deficit in dermato-mycological training. The overprescription of corticosteroids exacerbates the problem by suppressing immune surveillance in the stratum corneum, permitting fungal persistence. Terbinafine remains the only fungicidal agent with adequate keratin affinity.
Rachel Wermager
January 10, 2026 AT 11:16Actually, the KOH prep has a sensitivity of only ~70% for dermatophytes and even lower for Candida - which is why culture and PCR are gold standards. Also, most OTC antifungals are fungistatic, not fungicidal. That’s why recurrence rates are so high. And no, probiotics don’t do squat for cutaneous Candida - that’s a myth pushed by wellness influencers.
Tom Swinton
January 11, 2026 AT 00:29I just want to say - if you’re reading this and you’ve been dealing with this for months, please don’t feel ashamed. I used to hide my athlete’s foot under socks and sandals all summer. I thought it was just ‘bad hygiene’ - turns out, I just didn’t know what I was dealing with. This post? It’s the kind of thing I wish I’d found five years ago. Thank you for making it clear, real, and kind.
Leonard Shit
January 12, 2026 AT 19:50lol i once put hydrocortisone on what i thought was a sunburn... turned out it was jock itch. my groin looked like a red alien had hatched there. thanks, internet advice. 🤦♂️
Gabrielle Panchev
January 13, 2026 AT 00:36Wait - you’re telling me that ‘natural remedies’ like apple cider vinegar aren’t scientifically proven to eradicate dermatophytes? Shocking. Who knew modern medicine had actual data? I mean, I’ve been soaking my feet in vinegar since 2012, and my toenails still look like they’re from a horror movie. Maybe… just maybe… the doctors were right all along? 🤔
Venkataramanan Viswanathan
January 13, 2026 AT 06:46In India, we call ringworm 'dhaman' - it's common in monsoon season. Many families use neem paste or turmeric. But truth is, if it doesn't improve in 7 days, you need medicine. No shame. Just science. And yes - wash clothes in hot water. Cold water does nothing. I learned this the hard way after infecting my whole family.
Saylor Frye
January 13, 2026 AT 23:12Interesting. But I'm pretty sure the real issue is that people don't have access to dermatologists. This is a privileged conversation. In rural areas, you get whatever’s in the local pharmacy - usually a steroid cream because it 'works faster.' The problem isn't ignorance - it's inequality.
Kelly Beck
January 14, 2026 AT 12:06YOU DID IT!! 🎉 This is the kind of post that changes lives. I had recurrent Candida for 3 years - tried everything. Then I started drying my skin like a pro, switched to cotton underwear, and used clotrimazole for the full 14 days. No more shame. No more hiding. I’m finally free. Thank you for the truth, the science, and the hope. 💕 You’re a legend.