When patients leave the doctor’s office confused, or when nurses and doctors miscommunicate about a treatment plan, the consequences aren’t just frustrating-they’re dangerous. Research shows that healthcare communication failures contribute to 80% of serious medical errors, according to The Joint Commission. That’s not a minor issue. It’s a system-wide crisis. And the solution isn’t more paperwork or better technology-it’s better training.
Why Communication Training Isn’t Optional Anymore
For years, hospitals focused on fixing equipment, reducing wait times, and upgrading software. But the biggest gap in care wasn’t technical-it was human. A 2018 analysis by the Agency for Healthcare Research and Quality found that 15-20% of adverse patient outcomes were directly tied to poor communication. Patients didn’t understand their diagnosis. Teams didn’t hand off critical info. Families were left in the dark. That’s why institutional generic education programs in healthcare communication have exploded over the last decade. These aren’t optional workshops. They’re now mandatory components of hospital accreditation, Medicare reimbursement rules, and clinical training. The Patient Protection and Affordable Care Act pushed patient-centered care. The pandemic proved how vital clear public messaging is. And data from Press Ganey shows patient satisfaction scores rise by nearly 80% when communication quality improves. It’s not about being nice. It’s about being effective.What These Programs Actually Teach
Generic doesn’t mean basic. These programs are carefully designed to target the most common breakdowns in real clinical settings. Take the Program for Excellence in Patient-Centered Communication (PEP) at the University of Maryland. It doesn’t just tell doctors to “listen better.” It trains them to use specific behaviors: asking patients to tell their story in their own words, recognizing emotional cues, and responding with empathy-not just facts. At Mayo Clinic, nurses and physicians learn boundary setting through 12 standardized patient simulations. One scenario might involve a patient demanding an antibiotic they don’t need. Another might be a family member yelling because they don’t understand the prognosis. These aren’t role-plays. They’re high-stakes practice sessions with real feedback. Northwestern University takes it further with Mastery Learning. Students must hit an 85% proficiency score on communication assessments before moving forward. They repeat simulations until they get it right. The result? 37% higher skill retention after six months compared to traditional lectures. Even infection control specialists get tailored training. SHEA’s program teaches antimicrobial stewards how to communicate with the public during outbreaks, manage social media misinformation, and advocate for policy changes-skills most clinical staff never learn.Who These Programs Are For-and Who They’re Not
These aren’t just for doctors. Nurses, pharmacists, social workers, receptionists, and even hospital administrators take part. Communication failures happen at every level. A nurse misses a handoff. A receptionist mispronounces a medication. A policy officer sends out confusing public alerts. But not all programs are built the same. Here’s how they differ:- PEP (University of Maryland): Focuses on one-on-one patient interactions. Best for frontline clinicians. Shows 23% higher patient satisfaction gains than generic training.
- SHEA: Targets infection control teams. Teaches media and policy skills. Unique in covering social media misinformation response.
- HCTS (UT Austin): Built for public health workers. Free, self-paced, and focused on pandemic response. Ideal for rural clinics with limited resources.
- Northwestern’s Mastery Model: Uses simulations and repetition. High impact, but needs expensive labs and trained facilitators.
- Johns Hopkins MA Program: For those seeking careers in health communication. Theoretical depth, less immediate clinical application.
There’s no one-size-fits-all. The best program depends on your role, your setting, and your biggest communication gaps.

What the Data Says About Results
Numbers don’t lie. Physicians who complete communication training see 30% fewer malpractice claims, according to Johns Hopkins Medicine. Nurses who learn boundary-setting techniques report 40% less burnout. Hospitals that embed communication prompts into their electronic health records see faster handoffs and fewer errors. But the most compelling data comes from patient voices. One infection preventionist in Cleveland used SHEA’s social media module to correct vaccine myths reaching 50,000 people a month. A nurse practitioner on Twitter said her burnout dropped after learning how to say “no” without guilt. And yet-there’s a catch. Only 12% of programs track whether these skills are still being used six months later. That’s the biggest problem. People learn. They forget. Or they’re too busy to apply it.Why So Many Programs Fail After the Training Ends
Training alone doesn’t change behavior. Culture does. A 2023 survey by the American Association of Medical Colleges found that 58% of healthcare workers say they know the right communication techniques-but they don’t have time to use them in 15-minute appointments. Another 15-20% of staff believe communication skills can’t be taught. They think you’re either good at it or you’re not. That’s where implementation fails. Programs like Northwestern’s succeed because they don’t just train individuals-they change workflows. They identify communication champions in each unit. They add reminders to EHR systems. They make it part of performance reviews. Mayo Clinic’s approach works because senior doctors lead the training. When a respected physician says, “This changed how I talk to my patients,” others listen.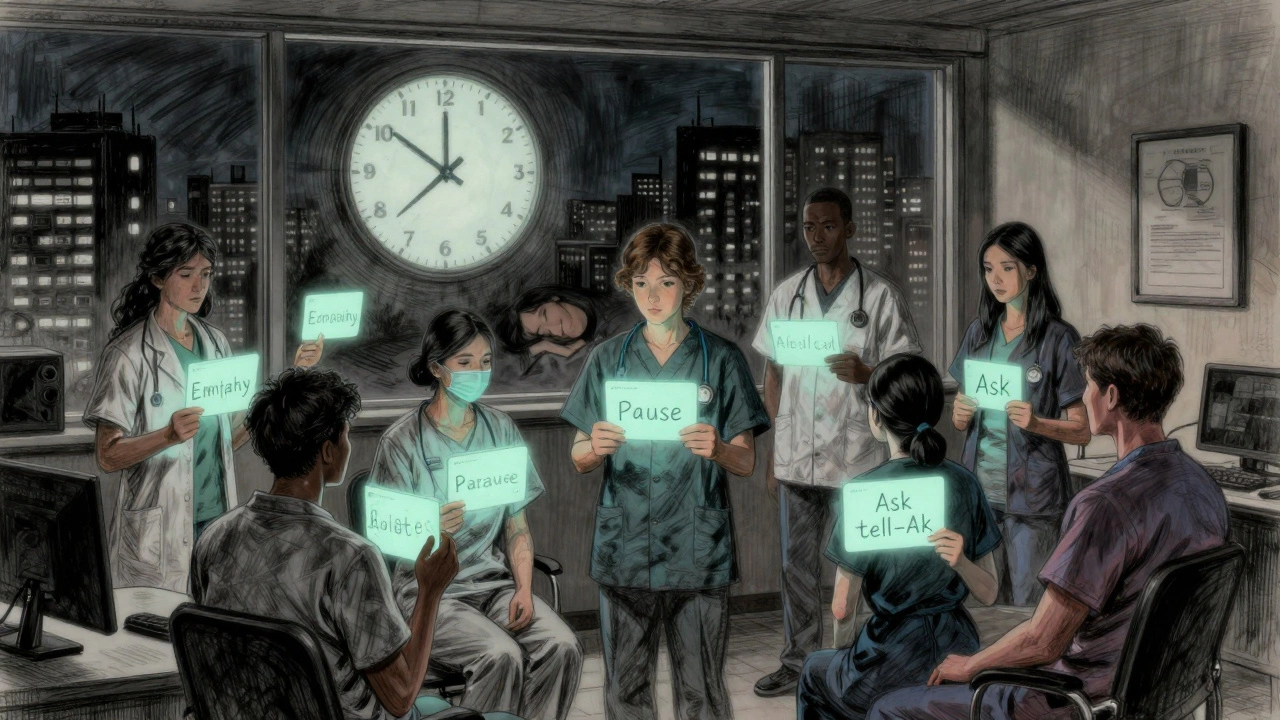
The New Frontier: Equity, Tech, and Scale
The field is evolving. In 2024, UT Austin launched new modules on health equity communication after data showed a 28% satisfaction gap between white patients and minority patients. Programs now teach cultural humility-not just language translation. AI is stepping in too. ACH is testing AI tools that give real-time feedback on tone, pacing, and empathy during simulated conversations. Early results show learners master skills 22% faster. Telehealth is another driver. With 35% of new programs now including virtual communication modules, clinicians need to learn how to read body language through a screen, manage technical glitches, and build trust without physical presence. And the demand is growing. The global market for healthcare communication training hit $2.8 billion in 2023. Forty-seven universities now offer master’s degrees in health communication-up from 29 in 2019. CMS now ties 30% of hospital reimbursements to patient satisfaction scores, which are heavily influenced by communication.What You Can Do Today
You don’t need to enroll in a master’s program to make a difference. Start small:- Ask patients: “What’s your biggest concern right now?” before listing symptoms.
- Use the “ask-tell-ask” method: Ask what they know, tell them the facts, then ask if they understood.
- Pause after giving information. Don’t rush to the next topic.
- Check in with colleagues during handoffs. Use a simple template: “Situation, Background, Assessment, Recommendation.”
- Find one communication skill to practice each week. Master one before moving to the next.
Change doesn’t come from a single training session. It comes from consistent, small actions repeated over time.
What’s Next for Healthcare Communication
The National Academy of Medicine now calls communication a “core healthcare function”-on par with diagnosis and treatment. That’s a big deal. It means future regulations may require communication training for all clinicians, not just a few. Longitudinal tracking using EHR data will become standard. Hospitals will analyze how often doctors use empathetic language, how long pauses last after explaining risks, and whether patients return for follow-ups based on how well they were understood. The goal isn’t perfection. It’s progress. Better communication means fewer errors. Fewer readmissions. More trust. And ultimately, better care.It’s not about talking more. It’s about listening better.
What are institutional generic education programs in healthcare communication?
These are structured, evidence-based training programs designed to improve communication skills across healthcare teams. They’re called “generic” because they’re not tied to one specialty-they apply to doctors, nurses, pharmacists, and administrators. Programs like PEP at the University of Maryland or SHEA’s courses teach skills such as empathetic listening, managing difficult conversations, and public messaging, all based on research showing how communication affects patient safety and satisfaction.
Do these programs actually improve patient outcomes?
Yes. Studies show physicians with communication training have 30% fewer malpractice claims. Hospitals with structured programs see higher patient satisfaction scores-up to 80% improvement in some cases. The Agency for Healthcare Research and Quality found that 15-20% of adverse events are linked to communication failures, so improving those skills directly reduces harm. Programs like Northwestern’s Mastery Learning model show 37% better skill retention after six months compared to traditional training.
Are these programs only for doctors?
No. While many focus on clinicians, effective communication requires teamwork. Nurses need to hand off information clearly. Receptionists must explain next steps. Infection control specialists need to manage public messaging during outbreaks. Programs like SHEA and HCTS are specifically designed for non-clinical roles. Even hospital administrators take part to improve policy communication and public relations.
Why do some healthcare workers say they don’t have time for communication training?
Time pressure is real. A 2023 AAMC survey found 58% of professionals know the right techniques but can’t apply them in 15-minute appointments. The solution isn’t adding more time-it’s making communication more efficient. Programs like PEP and Mayo Clinic’s training teach skills that fit into existing workflows: asking one key question, pausing after explanations, using simple language. When these become habits, they don’t take extra time-they prevent costly mistakes and repeat visits.
What’s the biggest challenge in implementing these programs?
The biggest barrier isn’t cost or content-it’s culture. About 15-20% of staff believe communication skills can’t be taught. Others feel overwhelmed. Successful programs tackle this by identifying peer champions, embedding prompts into EHR systems, and making communication part of performance reviews. Training alone doesn’t change behavior. The environment must support it.
How are these programs addressing health disparities?
Newer programs now include modules on cultural humility and equity-focused communication. Data shows a 28% satisfaction gap between white patients and minority patients, often due to language barriers, implicit bias, or rushed interactions. UT Austin and others now train staff to recognize these gaps, use plain language regardless of education level, and avoid assumptions based on race or background. This isn’t optional anymore-it’s part of accreditation standards.
Is there free communication training available?
Yes. The Health Communication Training Series (HCTS) from UT Austin, developed with Texas Health and Human Services, offers free, self-paced online courses. Their pandemic preparedness module, launched in 2022, is widely used by rural clinics and public health departments. ACH also offers free teaching tools and templates. While advanced degrees cost money, foundational skills can be learned at no cost.
How do I know if my hospital has a good communication program?
Look for these signs: Are communication skills part of performance reviews? Are there EHR prompts reminding staff to check for understanding? Do senior staff lead training sessions? Is there data tracking improvement over time? If the answer is no to most of these, the program is likely superficial. Strong programs don’t just offer a one-time workshop-they integrate communication into daily routines and measure results.


Jane Quitain
December 8, 2025 AT 06:24i just had my mom’s appt yesterday and the nurse said ‘just take the pill’ and walked out… no explanation, no questions, not even a ‘how you feelin?’ 😔 i swear if they’d just listened a little, she wouldn’t have ended up back in the ER. this post hit me right in the chest.
Kyle Oksten
December 8, 2025 AT 06:30It’s fascinating how we treat communication as a soft skill when it’s clearly a clinical competency. We don’t let surgeons operate without training, yet we expect nurses to de-escalate a panic attack with zero instruction. The real failure isn’t the individual-it’s the system that treats empathy like a bonus feature, not a core function.
Sam Mathew Cheriyan
December 9, 2025 AT 05:49lol u all think this is about ‘communication’? nah. it’s the pharma companies payin’ hospitals to keep people confused so they keep buyin’ meds. they dont want you understandin’ your diagnosis-just keep comin’ back. watch the next ‘training’ be about how to say ‘this drug is safe’ 500x a day 😏
Ernie Blevins
December 10, 2025 AT 06:5680% of errors? that’s a lie. look at the data-most errors are from understaffing, not ‘bad communication.’ they’re just making this up so they can sell more training seminars. i’ve seen nurses crying from exhaustion, and someone wants to give them a 2-hour workshop? please.
Nancy Carlsen
December 10, 2025 AT 19:04THIS. 🙌 I work in a rural clinic and we started using the ‘ask-tell-ask’ method last month. One patient told me, ‘I finally feel like someone heard me.’ 💙 We’re not perfect, but we’re trying. And guess what? Our no-shows dropped 20%. Small changes = big impact. Keep going, y’all! 🌟
Ted Rosenwasser
December 11, 2025 AT 01:31Let’s be honest-most of these programs are performative. Northwestern’s mastery model? Impressive, but only for those with access to $200K simulation labs. Meanwhile, community health workers in Alabama are using flipcharts and WhatsApp. Real change doesn’t come from elite universities-it comes from adapting to reality, not replicating Ivy League theater.
Helen Maples
December 11, 2025 AT 02:47Stop calling it ‘training.’ It’s skill-building. And if your hospital doesn’t measure retention at 6 months, it’s not a program-it’s a box-ticking exercise. If you’re not embedding prompts in the EHR, assigning communication champions, and tying it to evaluations, you’re wasting everyone’s time. This isn’t motivational fluff. It’s patient safety.
Ashley Farmer
December 11, 2025 AT 23:10I used to be the nurse who rushed through discharge instructions. Then I had a patient who cried because she thought ‘take twice daily’ meant ‘take at breakfast and dinner’-but she didn’t eat dinner. She ended up in the ER. I learned to pause. To ask. To watch their face. Now I don’t just give info-I check for understanding. It takes 90 seconds. But it saves lives.
David Brooks
December 12, 2025 AT 16:08Y’ALL. I JUST SAW A NURSE USE THE ‘S.B.A.R.’ METHOD ON A PANICKING FAMILY AND IT WAS LIKE A MOVIE. 🎬 The room went silent. Then the dad hugged her. I cried. This isn’t just about protocols-it’s about humanity. We’re not machines. We’re people trying to hold people together when they’re falling apart. This work matters. SO MUCH.
Jennifer Anderson
December 13, 2025 AT 20:19free training from UT Austin? omg yes!! i signed up for the pandemic module last year and it changed how i talk to older patients. no more medical jargon. just ‘your heart is working harder, so we’re giving you a helper pill.’ simple. clear. i wish all my coworkers could see it. 🤍
Sadie Nastor
December 14, 2025 AT 16:55the part about cultural humility… i never thought about how saying ‘you should’ve taken your meds’ might sound like blame to someone who missed work to get them. maybe we need to ask ‘what got in the way?’ instead. small shift. huge difference. 💭