IC Symptom Tracker & Management Assistant
Track Your Symptoms
Your Progress
Trending Triggers
Your symptoms are most commonly triggered by caffeine and stress according to your entries.
When you hear the term interstitial cystitis, you might picture chronic bladder pain, but many people don’t realize it often makes it hard to pee. If you’ve ever felt a sudden urgency, a weak stream, or have to strain to finish, that could be IC pulling the strings. This guide walks through why IC messes with your bathroom routine, how to spot the signs, and what you can actually do about it.
What Is Interstitial Cystitis?
Interstitial Cystitis is a chronic bladder condition characterized by pelvic pain, pressure, and a persistent urge to urinate without infection or obvious cause. It affects roughly 1 in 100 women and 1 in 1,000 men in the UK, and the symptoms can range from mild discomfort to debilitating pain. The exact cause is still a mystery, but researchers point to a leaky bladder lining, nerve over‑activity, and immune system quirks.
What Does “Difficulty Urinating” Mean?
Difficulty urinating describes any trouble getting urine out of the bladder. It can look like a weak stream, a feeling of incomplete emptying, frequent dribbling, or the need to push hard to start the flow. While occasional hiccups happen to anyone, chronic difficulty often signals an underlying issue-IC being a leading suspect.
How IC Causes Urinary Trouble
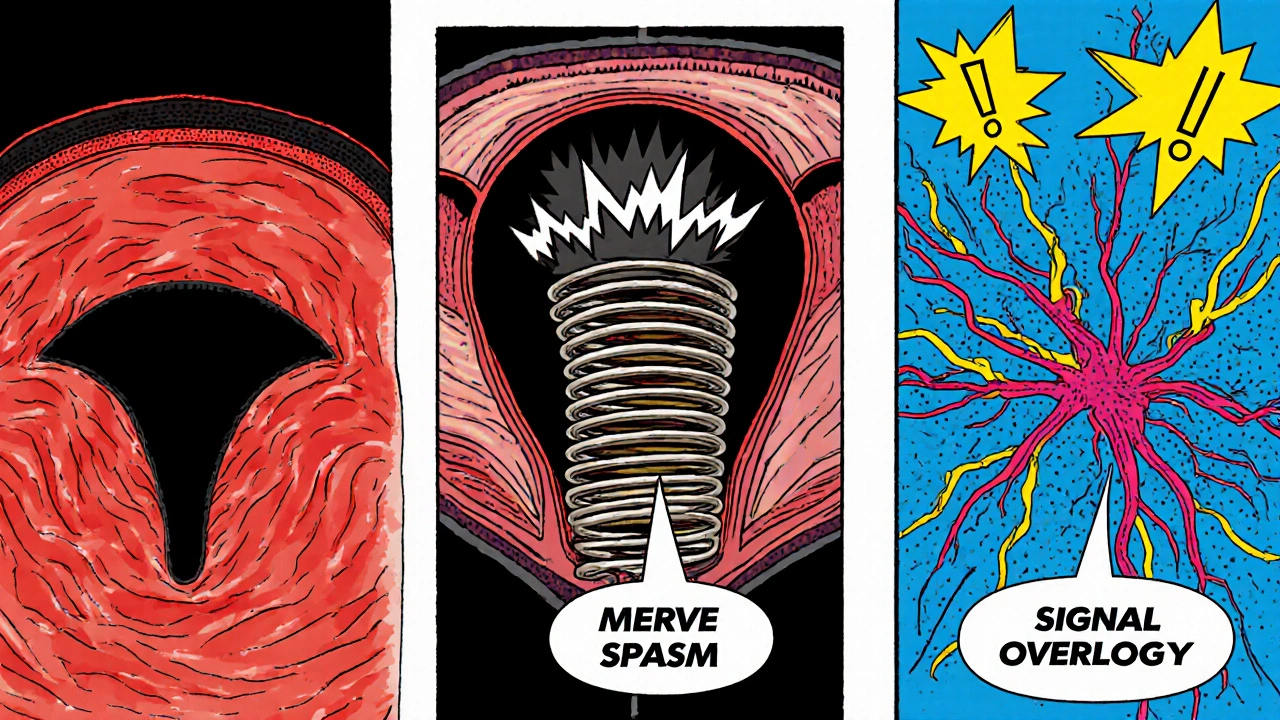
IC doesn’t just sit quietly in the bladder; it shakes up several systems that control peeing:
- Bladder wall inflammation: Swollen tissue narrows the opening (urethra), making the stream weaker.
- Pain‑driven muscle spasm: The pelvic floor muscles tighten to protect a sore bladder, which can block urine flow.
- Signal overload: Nerves send false urgency signals, so you feel you have to go even when the bladder isn’t full.
- Reduced bladder capacity: A chronically irritated bladder holds less urine, forcing you to go more often but with smaller amounts each time.
These factors often overlap, creating a perfect storm where you feel both urgency and a weak stream.
Symptoms Overlap: IC vs. Other Urinary Issues
| Feature | Interstitial Cystitis | Urinary Tract Infection (UTI) | Overactive Bladder (OAB) |
|---|---|---|---|
| Pain location | Deep pelvic or bladder pain, worsens when bladder fills | Burning during or after urination | Usually no pain |
| Urine test | Negative for bacteria | Positive for bacteria | Negative for bacteria |
| Urgency | Strong, often with pain | Frequent, sometimes with pain | Very frequent, no pain |
| Stream strength | Often weak or intermittent | Usually normal | Normal |
| Response to antibiotics | None | Improves quickly | No effect |
If you see a mix of these signs-especially pain without bacteria-IC could be the cause.
How Doctors Diagnose the Link
Getting a proper diagnosis means ruling out infections and other bladder disorders. Typical steps include:
- Medical history review-focus on pain patterns, diet, and previous pelvic issues.
- Urine analysis-to eliminate infection.
- Cystoscopy-using a tiny camera to look inside the bladder; doctors may notice tiny lesions called Hunner’s ulcers.
- Pelvic floor assessment-physiotherapists test muscle tension that could be contributing to difficulty urinating.
In some clinics, a bladder‑filling test (urodynamics) measures flow rates and capacity, giving concrete numbers on how IC is affecting your stream.
Management Strategies That Really Help
There’s no one‑size‑fit‑all cure, but several approaches tackle the root causes of urinary difficulty:
- Dietary tweaks: Cut back on acidic foods, caffeine, alcohol, and artificial sweeteners-these can irritate the bladder lining.
- Pain‑targeted meds: Oral antihistamines (e.g., hydroxyzine) and low‑dose tricyclic antidepressants (e.g., amitriptyline) calm nerve over‑activity.
- Bladder instillations: A gentle solution of dimethyl sulfoxide (DMSO) or heparin placed directly into the bladder can reduce inflammation.
- Pelvic floor physical therapy: Trained therapists teach relaxation techniques, biofeedback, and gentle stretching to unblock the urethra.
- Stress‑management: Mind‑body practices-yoga, meditation, CBT-lower overall pain perception and can improve urinary flow.
For severe cases where symptoms don’t improve, doctors may discuss nerve stimulation (sacral neuromodulation) or, rarely, bladder augmentation surgery.
When to Seek Medical Help
If you notice any of the following, book an appointment:
- Persistent pelvic pain lasting more than three weeks.
- Weak or intermittent urine stream combined with burning.
- Frequent nighttime trips to the bathroom (more than twice).
- Blood in urine or a sudden change in urine color.
Early diagnosis cuts down on trial‑and‑error treatments and helps you regain control over bathroom habits.
Quick Checklist for Living with IC‑Related Urinary Issues
- Track symptoms in a diary-note pain level, stream strength, foods, and stress triggers.
- Stay hydrated, but sip water throughout the day rather than gulping large amounts.
- Avoid bladder irritants (caffeine, citrus, spicy foods).
- Practice pelvic floor relaxation-gentle breathing exercises before and after using the toilet.
- Follow up with your urologist every 6‑12 months even if symptoms improve.
Frequently Asked Questions
Can interstitial cystitis cause urinary retention?
Yes. Inflammation and pelvic floor spasm can block the urethra enough that the bladder doesn’t empty completely, leading to retention.
Is it normal to have a weak stream with IC?
A weak or intermittent stream is common because the inflamed bladder wall can restrict the flow and the pelvic muscles may contract unintentionally.
Do antibiotics help if I have difficulty urinating?
Only if a bacterial infection is present. Since IC is non‑infectious, antibiotics won’t relieve the symptoms and may cause resistance.
Can lifestyle changes reduce my symptoms?
Absolutely. Cutting bladder irritants, staying hydrated, and doing pelvic floor relaxation exercises have been shown to improve both pain and urinary flow for many patients.
Is there a cure for interstitial cystitis?
A definitive cure remains elusive, but a combination of diet, medication, and physical therapy can manage symptoms effectively for most people.
Understanding the link between interstitial cystitis and difficulty urinating empowers you to spot the signs early, get the right tests, and start a treatment plan that actually works. You don’t have to live with constant pain and bathroom hassles-take the first step by talking to a urologist or a specialised pelvic health therapist today.


diego suarez
October 16, 2025 AT 17:22It’s interesting how the bladder’s lining can become so permeable that it starts sending mixed signals to the brain. When the wall inflames, the urethral opening may shrink a bit, which explains that weak stream many people notice. On top of that, chronic pain often makes the pelvic floor tighten, acting like a gatekeeper that blocks urine flow. Keeping a symptom diary can help you spot patterns without jumping to conclusions.
Abhishek A Mishra
October 17, 2025 AT 10:02i totally get the frustration when you have to push like a marathon runner just to start peeing. cutting back on coffee and soda can actually calm the bladder nerves a lot more than you think. also, try sipping water throughout the day instead of gulping a bucket at once – it keeps the flow steadier. staying consistent with pelvic floor stretches might make a real difference.
Jaylynn Bachant
October 18, 2025 AT 02:42the body, in its quiet wisdom, sometimes whispers through pain that something is amiss. when the bladder’s tiny walls leak, the mind receives false urgency, like a siren that never stops. this paradox of feeling full while the reservoir is nearly empty can be baffling, yet it nudges us toward deeper self‑care. honoring those signals with gentle breath work may ease the muscle spasm that blocks the stream.
Becky B
October 18, 2025 AT 19:22While many health guides focus on diet and meds, it’s worth noting that some pharmaceutical studies on interstitial cystitis have been quietly funded by interests that downplay natural therapies. In the U.S., regulatory oversight sometimes favors large drug manufacturers, leading patients to chase expensive prescriptions that barely address the underlying muscle tension. Exploring pelvic floor physiotherapy-often overlooked by mainstream clinics-can provide a non‑pharmaceutical path to regaining control of your urine flow.
Aman Vaid
October 19, 2025 AT 12:02From a physiological standpoint, the interplay between bladder wall inflammation and urethral sphincter tone is central to the presentation of a weak urinary stream in IC patients. Histological analyses have demonstrated that mast cell activation contributes to the release of proteases, which degrade the glycosaminoglycan layer and increase urothelial permeability. Consequently, afferent nerves become hypersensitive, generating premature urgency signals. Moreover, chronic pelvic floor hypertonicity can mechanically obstruct the outflow, reinforcing the sensation of incomplete emptying.
Dominic Ferraro
October 20, 2025 AT 04:42That’s a solid breakdown-thanks for the detail! Knowing the exact mechanisms makes it easier to target treatment. A good next step is to combine bladder‑instillation therapy with pelvic floor relaxation exercises to attack both the inflammation and the muscle spasm.
Jessica Homet
October 20, 2025 AT 21:22Honestly, most of the “miracle diet” advice out there feels like marketing fluff. Cutting caffeine helps, but the real game‑changer is consistent pelvic floor physical therapy, which many urologists still dismiss. If you’re not seeing improvement after a month of meds, push for a qualified therapist who can teach you proper relaxation techniques.
mitch giezeman
October 21, 2025 AT 14:02For anyone dealing with a weak stream, I’d suggest starting with a simple bladder‑training schedule: set timed bathroom trips every two to three hours, even if you don’t feel the urge. Pair that with a gentle warm sitz bath after each session to relax the pelvic muscles. Over a few weeks you’ll often notice a steadier flow and less urgency.
Kelly Gibbs
October 22, 2025 AT 06:42I’ve seen a few folks mention that staying hydrated throughout the day, rather than drinking large volumes at once, can reduce the frequency of sudden urges. It’s a small habit change that sometimes makes a noticeable difference in stream strength.
Bailey Granstrom
October 22, 2025 AT 23:22Stop ignoring the pain-your bladder isn’t a joke.
inas raman
October 23, 2025 AT 16:02Totally agree with the sitz bath tip! Adding a few minutes of diaphragmatic breathing while you’re in the tub can really melt away that pelvic tension and help the urine flow smoother.
Anne Snyder
October 24, 2025 AT 08:42When examining the pathophysiology of interstitial cystitis‑related urinary dysfunction, it is essential to integrate both neurogenic and myogenic components into a cohesive treatment algorithm. First, the disruption of the glycosaminoglycan (GAG) layer facilitates urothelial permeability, which in turn precipitates a cascade of inflammatory mediators such as cytokines, prostaglandins, and neuropeptides. These mediators sensitize afferent C‑fibers, lowering the threshold for urgency signals and creating a false perception of bladder fullness. Simultaneously, chronic nociceptive input induces hypertonicity of the levator ani and external urethral sphincter, effectively imposing a functional outflow obstruction. Clinical studies have demonstrated that targeted pelvic floor physical therapy can reduce sphincteric pressure by up to 30%, thereby ameliorating weak stream phenomena. Moreover, oral antihistamines such as hydroxyzine function as mast cell stabilizers, attenuating the release of histamine and tryptase that exacerbate mucosal irritation. Intravesical instillation of dimethyl sulfoxide (DMSO) provides an additional anti‑inflammatory vector by directly solubilizing inflammatory debris within the bladder lumen. It is also prudent to incorporate neuromodulatory interventions, such as sacral nerve stimulation, for refractory cases where peripheral desensitization fails to yield symptomatic relief. Nutritional modulation-specifically the elimination of acidic foods, caffeine, and artificial sweeteners-serves to reduce GAG layer degradation and may synergize with pharmacologic agents. Patients should be encouraged to maintain a bladder diary, documenting fluid intake, voiding intervals, stream quality, and pain scores, as this data informs iterative adjustments to the therapeutic regimen. Stress reduction techniques, including mindfulness‑based stress reduction (MBSR) and guided imagery, have been shown to down‑regulate the hypothalamic‑pituitary‑adrenal axis, consequently diminishing pro‑inflammatory cytokine production. In practice, a multimodal approach that sequentially addresses urothelial integrity, neural hypersensitivity, and pelvic floor mechanics yields the most robust improvement in urinary flow dynamics. Finally, regular follow‑up with a multidisciplinary team-comprising urologists, physiatrists, and pelvic‑health physiotherapists-ensures that treatment efficacy is continually evaluated and optimized. Adherence to the prescribed regimen is critical, as inconsistent therapy can lead to symptom relapse. By embracing this comprehensive, evidence‑based framework, individuals with IC can reclaim functional bladder control and experience a substantial reduction in urinary distress.
Rebecca M
October 25, 2025 AT 01:22While the content is comprehensive, note the inconsistent use of the em‑dash-sometimes it appears without surrounding spaces, which can disrupt readability; additionally, “hypertonicity” should be hyphenated as “hyper‑tonicity” for clarity, and “pelvic health physiotherapists” might be better rendered as “pelvic‑health physiotherapists.” These minor edits will enhance the professional polish of the piece.