Every year, thousands of children in the U.S. and UK receive the wrong dose of medicine-not because someone was careless, but because a simple number was off. A child weighing 12 kg gets a dose meant for a 25 kg child. A caregiver misreads pounds as kilograms. A nurse administers liquid medicine based on an old weight entry from three weeks ago. These aren’t hypotheticals. They’re real, preventable mistakes that land kids in emergency rooms, and sometimes worse.
The solution isn’t more training or better memory. It’s a system built around one critical fact: pediatric dosing is weight-based. Get the weight right, and you cut the risk of error by more than half. Get it wrong, and even the most experienced pharmacist or nurse can make a deadly mistake.
Why Weight Is the Most Important Number in Pediatric Pharmacy
Adults usually get fixed doses: one tablet, one vial, one teaspoon. Kids don’t. Their bodies process medicine differently. A dose that’s safe for a 10-year-old could kill a 6-month-old. That’s why pediatric medications are almost always calculated in milligrams per kilogram (mg/kg) or milligrams per square meter (mg/m²). It’s precise. It’s scientific. And it’s unforgiving if the weight is wrong.
According to the World Health Organization, children are three times more likely to suffer a medication error than adults. The biggest reason? Weight conversion mistakes. In one study, 32.7% of all pediatric dispensing errors involved incorrect weight-based calculations. Nearly 9 out of 10 of those errors happened because someone used pounds instead of kilograms-or the weight in the system was outdated.
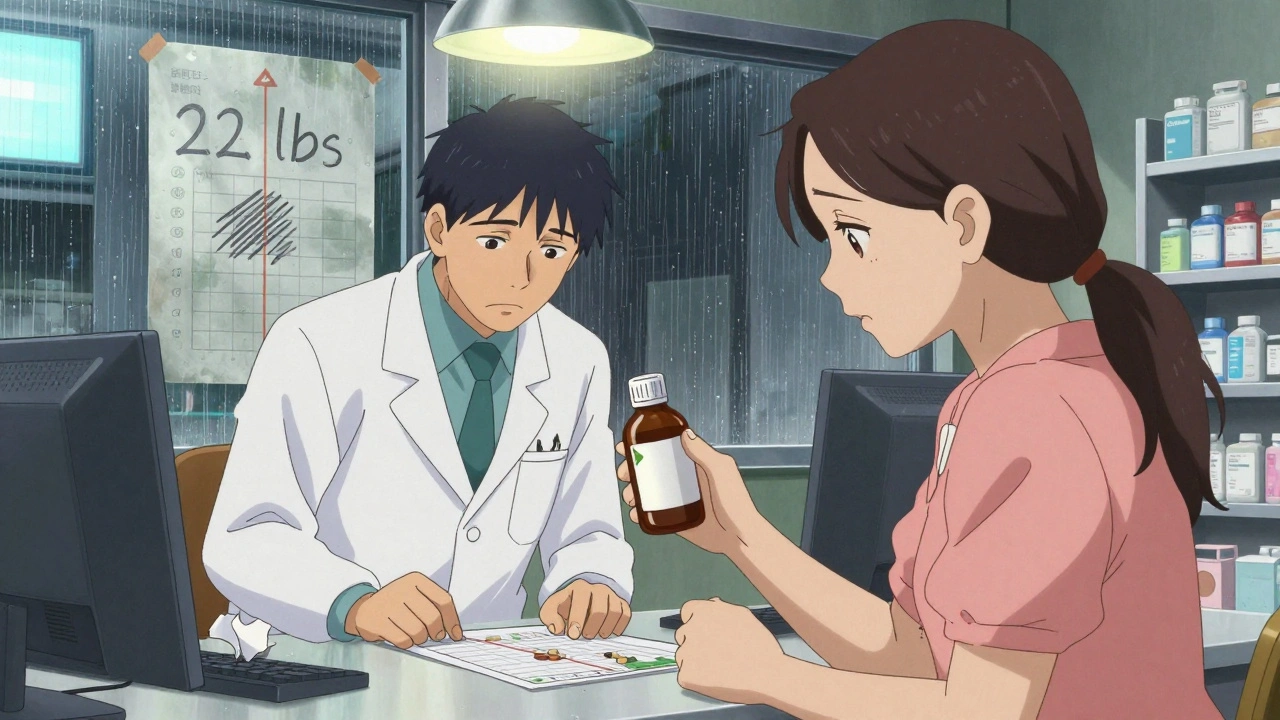
Think about it: if a child weighs 22 pounds and the system shows 22 kilograms, that’s a 100% overdose. That’s not a typo. That’s a crisis.
How Weight-Based Verification Systems Work
A weight-based verification system isn’t just a pop-up alert. It’s a chain of checks that must happen every single time a child gets medicine. Here’s how it works in the best-run hospitals and pharmacies:
- Weight is measured in kilograms only. No pounds. No ounces. Digital scales must display only kilograms-with precision to 0.1 kg for infants and 0.5 kg for older children. This eliminates the most common source of error: manual conversion.
- Weight must be entered before any prescription can be submitted. Electronic health records (EHRs) are configured to block order entry unless a current weight is in the system. No weight? No order.
- The system calculates the dose automatically. Once weight is entered, the EHR uses built-in dosing rules to suggest the correct amount. If the prescriber enters a dose outside the safe range, the system flags it with a warning.
- Pharmacists verify every calculation. Even with automation, a pharmacist must review the dose, confirm the weight, and sign off. This isn’t optional. It’s the last safety net.
- Barcode scanning at the bedside confirms weight and dose. Before the medicine is given, the nurse scans the child’s wristband, the medication, and the dose. If the weight doesn’t match the expected range, the system stops the administration.
This isn’t science fiction. It’s standard practice in top children’s hospitals. At Boston Children’s Hospital, after implementing this full system, weight-related errors dropped from 14.3 per 10,000 doses to just 0.8-over a 94% reduction.
The Tools That Make It Possible
You can’t do this with paper charts and mental math. You need technology-but not just any technology. The right tools are designed specifically for pediatric safety.
- Electronic Health Records (EHRs) with Clinical Decision Support (CDSS): Systems like Epic and Cerner now have pediatric-specific modules. They know that a 10 mg dose of morphine for a 5 kg infant is dangerous. They flag it before it’s written.
- Automated Dispensing Cabinets (ADCs): These are the drug drawers in hospital units. When a nurse pulls a pediatric medication, the cabinet checks the patient’s weight against the dose. If it doesn’t match, the drawer won’t open.
- Barcode Medication Administration (BCMA): This system links the child’s ID, the drug, the dose, and the weight. If any piece doesn’t fit, the system won’t let the medication be given.
- Standardized Concentrations: Instead of having 5 different strengths of amoxicillin, hospitals now standardize to one concentration-say, 25 mg/mL. That means less calculation, fewer errors.
One study found that hospitals using standardized concentrations reduced calculation errors by 72.4%. Simple change. Huge impact.
Why Some Systems Fail-And How to Fix It
Not every hospital gets it right. Even with the best tech, systems fail when people bypass them or when the data is stale.
Here’s what goes wrong:
- Alert fatigue: If the system flags every dose over 10 kg as “possible overdose,” clinicians start ignoring it. A 2021 study found 41.7% of weight-based alerts were overridden-and 18.3% of those overrides were actual errors.
- Outdated weights: A child’s weight can change fast. A 12-month-old who weighed 9 kg in January might weigh 10.5 kg by March. If the system still shows 9 kg, the dose is wrong. The Institute for Safe Medication Practices says: “Weights must be measured within 24 hours for inpatients and within 30 days for outpatients.”
- Community pharmacies are left behind: Most community pharmacists don’t have access to the child’s EHR. They rely on what the parent says-or what’s printed on the prescription. A 2023 survey found that 28.4% of community pharmacists had a near-miss due to incorrect weight in the past month.
- Training gaps: Many nurses and doctors were never taught pediatric pharmacokinetics. They know how to dose an adult. They don’t know how to adjust for a 3-month-old’s liver metabolism.
The fix? Three things:
- Make weight entry mandatory at every point of contact. No exceptions.
- Train every staff member on pediatric dosing. Not just pharmacists. Nurses, physicians, even receptionists who weigh kids at check-in.
- Use smart alerts. Newer systems like Epic’s Pediatric Safety Module 4.0 don’t just check weight-they check if the dose makes sense for the child’s age and growth percentile. That cuts false alarms by over 60%.
The Real Cost of Getting It Wrong
It’s easy to think, “It’s just a typo.” But the consequences aren’t abstract.
A child given too much acetaminophen can suffer liver failure. Too much morphine can stop breathing. Too little antibiotics can turn a simple ear infection into sepsis. A 2021 review found that 8.4% of pediatric dosing errors caused measurable harm-some permanent, some fatal.
And it’s not just the child. It’s the family. It’s the nurse who has to explain what happened. It’s the pharmacist who loses sleep over a mistake they didn’t see coming.
The financial cost is high too. Medication errors add $4.4 billion annually to U.S. healthcare costs. But the human cost? That’s unquantifiable.
What You Can Do-Even If You’re Not in a Hospital
You don’t have to work in a children’s hospital to help prevent these errors. If you’re a parent, caregiver, or even a community pharmacist, here’s what you can do:
- Always ask: “What’s the child’s weight in kilograms?” If they say pounds, convert it yourself: divide by 2.2.
- Check the label. Is the dose listed in milliliters (mL)? If it’s in teaspoons or tablespoons, that’s a red flag. Liquid pediatric meds should only be measured in mL.
- Ask the pharmacist to double-check the dose. Say: “Can you confirm this dose is right for their weight?” Most pharmacists will be glad to.
- Update weight regularly. If your child is seeing a doctor every few months, make sure their weight is recorded each time. Don’t assume they remember.
Even small actions add up. One parent who asked for a weight check prevented a 3x overdose of amoxicillin. That’s not luck. That’s vigilance.
The Future Is Smarter-But Still Human
Technology is getting better. The FDA is pushing for EHRs to integrate growth charts so they can predict a child’s expected weight. AI is being tested to flag weights that don’t match age or height. Blockchain is being explored to lock weight data so it can’t be altered.
But none of this matters if the culture doesn’t change. As Dr. Robert Wachter from UCSF says: “Technology alone cannot prevent errors; a culture of safety with non-punitive error reporting is essential.”
That means: if a nurse catches a wrong dose, they shouldn’t fear blame. They should be thanked. If a pharmacist notices a weight is outdated, they should be empowered to stop the process. If a parent questions a dose, they should be heard-not dismissed.
Preventing pediatric dispensing errors isn’t about having the fanciest system. It’s about making sure every person in the chain-doctor, nurse, pharmacist, parent-knows that weight isn’t just a number. It’s the difference between healing and harm.
Why is weight so important in pediatric dosing?
Children’s bodies process medicine differently than adults. Doses are calculated based on weight in kilograms (mg/kg), not fixed amounts. A small change in weight can mean a dangerous change in dose. A 5 kg infant needs far less than a 20 kg child-even for the same condition.
What’s the most common cause of pediatric dosing errors?
The most common cause is weight conversion errors-especially when pounds are mistaken for kilograms. Other top causes include outdated weight entries in medical records and incorrect manual calculations. About 12.6% of errors come from using pounds instead of kilograms.
Can I trust the weight in my child’s medical record?
Not always. Studies show 63% of pediatric nurses have seen weight documentation errors in the past year. Always confirm the current weight before any medication is given. If your child hasn’t been weighed in over 30 days, ask for a new measurement.
Should liquid pediatric medications be measured in teaspoons or milliliters?
Always in milliliters (mL). Teaspoons and tablespoons vary in size and are too imprecise for children. The American Academy of Pediatrics mandates that all pediatric liquid medications be labeled and dispensed in mL only.
What should I do if I think my child’s dose is wrong?
Stop. Don’t give the medication. Call the pharmacy or prescribing provider and say: “Can you confirm this dose is correct for my child’s current weight?” Most professionals welcome this question. It’s your right-and it could save your child’s life.
Preventing pediatric dispensing errors isn’t a one-time fix. It’s a daily habit-of measuring, verifying, questioning, and double-checking. Every weight entered, every dose confirmed, every question asked adds up to a safer system. And for children, that’s not just good practice. It’s essential.


patrick sui
December 3, 2025 AT 02:14Massive props to the author for breaking this down. The mg/kg paradigm is non-negotiable - I’ve seen nurses eyeball doses because ‘the kid looks about 15 kg’ 😬. Weight isn’t a suggestion, it’s the cornerstone. And yes, standardized concentrations? Absolute game-changer. No more ‘is this 125 or 250 mg/mL?’ confusion. Epic’s CDSS flags are still too noisy, but they’re getting better. 👍
Conor Forde
December 5, 2025 AT 01:11So let me get this straight - we’re now treating kids like rockets that need a 14-step launch sequence just to get a cough syrup? 🤦♂️ Next they’ll scan your kid’s DNA before giving them Tylenol. Look, I get it - mistakes happen. But this is over-engineering the crap out of a system that’s been fine for decades. Parents used to mix doses with a kitchen spoon and the kid lived. Now we need blockchain and AI to stop a typo? 😅
Declan O Reilly
December 6, 2025 AT 07:05There’s something deeply human here - we’re not just preventing errors, we’re rebuilding trust. Every time a nurse stops to verify weight, they’re saying: ‘I see you. You matter.’ That’s the real tech. Not the barcode scanner. Not the EHR. It’s the moment someone pauses, breathes, and says ‘Let me check again.’ That’s where healing happens. And yeah, maybe we’ve made it too complicated… but if complexity saves one child’s liver, isn’t it worth it? 🙏
Matt Dean
December 7, 2025 AT 10:09Wow. Just… wow. This is the kind of post that makes me want to cry because it’s so obvious and yet so ignored. You want to know why kids die from medication errors? Because hospitals treat weight like a suggestion, not a law. And pharmacists? They’re overworked, underpaid, and expected to be human calculators. This isn’t a ‘system failure’ - it’s a moral failure. Fix the culture first. The tech will follow. Stop blaming the tools. Blame the people who let the tools rot.
Walker Alvey
December 7, 2025 AT 23:46Of course the solution is more tech. Because nothing says ‘safety’ like a computer telling a nurse what to do. Next they’ll install a drone to deliver the medicine and a therapist to console the nurse after she’s forced to follow the algorithm. Meanwhile, the kid who got 3x the dose because the mom said ‘he’s about 30 pounds’ is now in ICU. But hey - at least the system didn’t flag it. Because it was ‘human error.’ Classic. 🙃
Michelle Smyth
December 9, 2025 AT 03:41It’s fascinating how the author reduces pediatric pharmacology to a spreadsheet. Weight-based dosing is a statistical artifact of Western biomedical hegemony. In many cultures, dosing is relational - tied to developmental stage, not mass. The obsession with kilograms is a colonial relic. And don’t get me started on Epic’s ‘Pediatric Safety Module’ - it’s just another corporate product wrapped in virtue signaling. The real solution? Abolish the EHR and return to clinical intuition. Or at least, stop pretending tech can replace judgment.
ANN JACOBS
December 10, 2025 AT 05:23I want to thank you for this incredibly thoughtful, comprehensive, and deeply necessary exploration of a crisis that is both systemic and deeply personal. The statistics are staggering - 32.7% of errors tied to weight miscalculations - and yet, we continue to treat this as an operational issue rather than a moral imperative. The fact that community pharmacies remain disconnected from pediatric EHRs is not just a technical gap - it is a failure of care equity. Every child, regardless of zip code or insurance status, deserves the same level of precision. We must advocate for interoperability, standardized training, and above all, the normalization of questioning. A parent’s doubt is not defiance - it is devotion. And we must honor that.
Courtney Co
December 10, 2025 AT 22:02My niece got the wrong dose last year because the clinic used her weight from 6 months ago. She ended up in the ER. I didn’t know what to do. I just kept asking ‘Are you sure?’ and they kept saying ‘It’s in the system.’ I felt so powerless. Now I carry her weight in my phone. I write it on the prescription. I ask the pharmacist to recalculate it out loud. I don’t care if I’m annoying. I’d rather be annoying than bury my child. If you’re reading this - do the same. Don’t wait for the system to fix itself. Be the glitch in the machine.
Shashank Vira
December 11, 2025 AT 04:47Let’s be honest - this entire framework is a Western luxury. In rural India, a child gets medicine based on age, appearance, and the pharmacist’s gut. And guess what? Most survive. Why? Because we don’t have the luxury of EHRs, barcode scanners, or 0.1 kg precision scales. We have love, experience, and shared community knowledge. You’re solving a problem that doesn’t exist in 80% of the world. This isn’t universal safety - it’s cultural imperialism disguised as innovation. 🤷♂️
Eric Vlach
December 11, 2025 AT 20:10Agreed on the weight thing. But why are we still using kg for infants? Most are under 10 kg - why not use grams? 10,000 g is way less ambiguous than 10 kg. And why do we still let nurses guess weights? I’ve seen them use the ‘look and guess’ method. We need scale integration at check-in. No exceptions. Also - stop calling it ‘pediatric.’ Just call it ‘child-safe dosing.’ It’s not a specialty. It’s basic.
Souvik Datta
December 12, 2025 AT 12:43Let me tell you something - I used to be a pharmacist in Mumbai. We didn’t have EHRs. We had handwritten scripts, parents who didn’t know their child’s weight, and no barcode scanners. But we had one rule: if you’re unsure, stop. Ask. Recalculate. Double-check. That’s the real system. Not the tech. The human pause. The courage to say ‘I need to verify.’ That’s what we lost. We outsourced responsibility to algorithms. And now we’re surprised when they fail. The answer isn’t more tech. It’s more courage.
Priyam Tomar
December 12, 2025 AT 13:33Everyone’s acting like this is new. It’s not. I’ve been in this field for 20 years. We’ve had weight-based alerts since the 90s. The problem isn’t the tech - it’s the people who override them. 18% of overrides were errors? That’s not a system flaw. That’s a workforce problem. Stop blaming Epic. Fire the nurses who ignore alerts. Train the ones who don’t. And for god’s sake, stop letting parents say ‘he’s about 30 pounds’ - make them weigh the kid. Every. Single. Time. No exceptions. That’s not overkill. That’s professionalism.
Jack Arscott
December 13, 2025 AT 03:53Just read this on my lunch break. 🥺 My cousin’s kid almost died from a 3x overdose because the weight was wrong. I didn’t know what to say. This post? It’s everything. Thank you. I’m printing this out and giving it to my sister. She’s a new mom. She needs to know it’s okay to ask. It’s not rude. It’s life-saving. 💙