Every year, hundreds of thousands of people in the U.S. end up in the hospital because of a simple mistake: they took the wrong pill, at the wrong time, or too much of it. For older adults managing five, ten, or even more medications, this isn’t just a risk-it’s a daily reality. The good news? You don’t need to live in fear. With the right system in place, you can cut the chance of a dangerous error by more than half.
Why Medication Mistakes Happen at Home
It’s easy to think, “I’ve been taking this for years, I know what I’m doing.” But the truth is, our brains aren’t wired to handle complex medication schedules. A 78-year-old with high blood pressure, diabetes, arthritis, and heart disease might be on eight different pills. Some need to be taken with food. Others must be spaced six hours apart. A few are only for when symptoms flare up. Mix in over-the-counter painkillers, vitamins, and herbal supplements, and the system starts to crack. According to the CDC, medication errors contribute to 22% of hospital readmissions after discharge. That’s not a small number. It’s not just about forgetting a dose-it’s about taking the wrong one, doubling up because you’re unsure, or mixing pills that shouldn’t be taken together. The consequences? Dizziness that leads to a fall. Confusion that turns into an ER visit. Kidney damage from too much NSAIDs. These aren’t hypotheticals. They happen every day.The Foundation: Your Medication List
The single most important step in medication safety? Writing down everything you take. Not just prescriptions. Not just the ones your doctor knows about. Everything. That daily aspirin. The turmeric supplement your cousin swore by. The antacid you take after dinner. The sleep aid you only use on weekends. Write them all down-name, dose, frequency, reason, and when you take them. Do this with your pharmacist or doctor. Don’t rely on memory. Bring your actual pill bottles to the appointment. Ask: “Is this still necessary?” “Could any of these interact?” “Is there a simpler way to take these?” Many people find out they’re taking duplicate medications or drugs that no longer help. This list isn’t a one-time task. Update it every time you get a new prescription, stop a medication, or try a new supplement. Keep a printed copy in your wallet and another on the fridge. Share it with your caregiver or family member who helps you manage your health.Choosing the Right Tool: From Pill Boxes to Smart Dispensers
Not every solution works for every person. Your needs depend on how many medications you take, how often you take them, and whether you live alone or have help nearby. Basic pill organizers (AM/PM boxes) cost $5 to $25. They’re cheap and simple. But they don’t remind you. They don’t track if you took your pill. If you’re sharp, independent, and on a simple routine-maybe just two pills a day-they’re fine. But if you’ve missed doses before, or if your memory isn’t what it used to be, this isn’t enough. Smart dispensers like Hero, MedMinder, or DosePacker are the next step. These are devices that hold your pills in labeled compartments and release them at preset times. When it’s time, they beep, flash lights, and send alerts to your phone. Some even let you talk to a pharmacist via video call right from the device. A 2022 NIH study found users of these devices had a 98% adherence rate over six months. That’s huge. Compare that to the 60-70% adherence rate seen in people who rely on alarms or paper lists. These devices also notify family members if you miss a dose. For caregivers, that peace of mind is priceless. The catch? They cost $150 to $300 upfront, plus $15 to $50 a month for service. Setup can take a few hours. You need Wi-Fi. And if your regimen changes-say, your doctor adds a new pill or removes one-you’ll need help reprogramming it. That’s where human support comes in.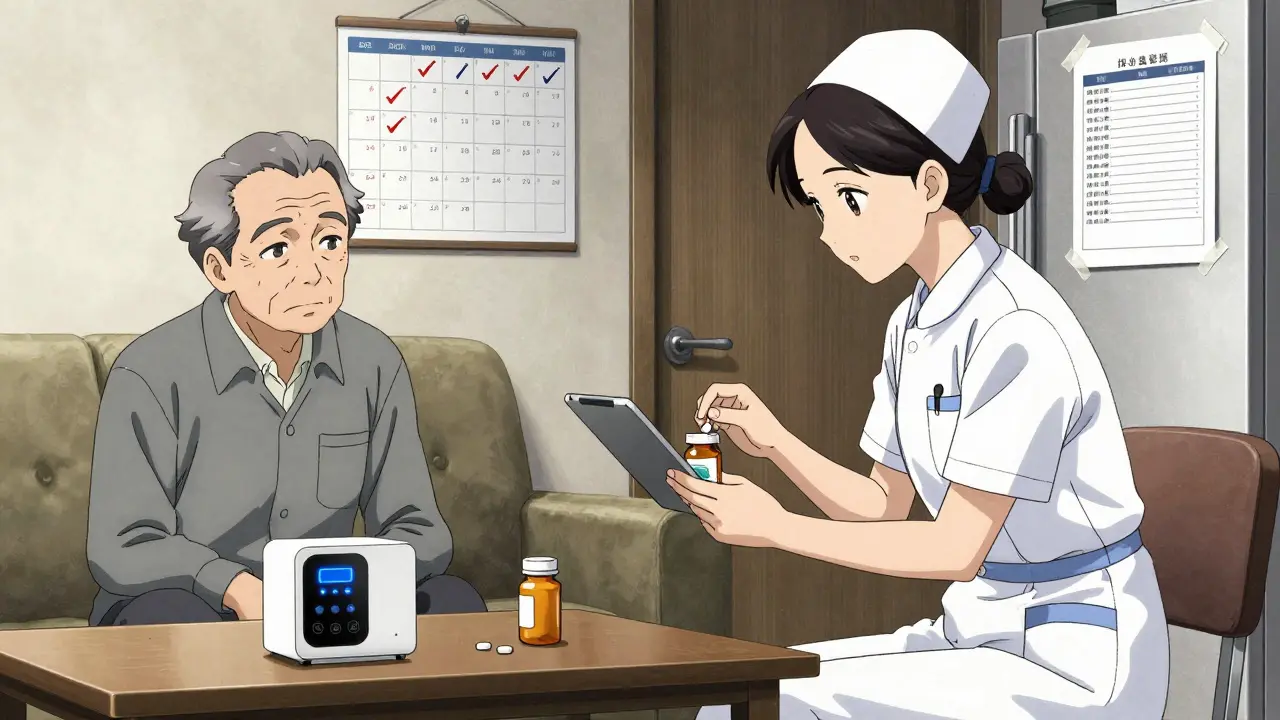
Digital Platforms: The Hidden Advantage
Beyond hardware, there are digital platforms like HomeMeds, launched in 2024 by the Partners in Care Foundation. These aren’t devices you buy-they’re apps and tools used by nurses and pharmacists during home visits. Here’s how they work: A clinician comes to your home with a tablet. You hand them your pill bottles. They scan each label with the camera. The app auto-fills your medication list, checks for interactions, flags duplicates, and even spots pills that are expired or running low. It cuts the time to assess your meds by 50%. The best part? It doesn’t just help you. It helps your care team. If your doctor sees you’ve been skipping your blood pressure pill, they can adjust your plan before you end up in the hospital. And in Fall 2025, HomeMeds will launch an AI version that can predict which medications are most likely to cause side effects like dizziness or confusion-two major causes of falls in older adults.Putting It All Together: Your No-Mistake System
A truly safe system isn’t one tool. It’s a combination of three things: a clear list, a reliable device, and human oversight. Here’s how to build it:- Make your master list-every pill, every supplement, every dose. Update it monthly.
- Choose a smart dispenser if you take more than three pills a day, or if you’ve missed doses before. Look for one with remote alerts and video support.
- Set up a check-in routine. Every 30 to 90 days, have a pharmacist or home health nurse review your list and device settings. Don’t wait until something goes wrong.
- Involve a caregiver. Even if you live alone, give someone access to the app or device alerts. They don’t need to be there every day-they just need to know if you’ve missed a dose.
- Keep backups. If the power goes out, your device won’t work. Keep a printed schedule and your pills in a labeled container as a backup.
What Doesn’t Work (And Why)
Not every solution is worth your time-or your money. Phone alarms alone? Too easy to ignore. Too easy to turn off. People in the Capterra survey said 41% of those who relied only on phone reminders still missed doses. Color-coded pill boxes? Helpful if you have good eyesight. Useless if you’re struggling with vision or dementia. Labels need to be large, clear, and readable-even in dim light. Just trusting your memory? That’s how most errors start. Your brain gets tired. You’re distracted. You’re in a hurry. You assume you took it. You didn’t. You take it again. Now you’ve doubled your dose. And here’s a big one: technology without support. A smart dispenser won’t help if you can’t figure out how to change the schedule when your doctor adds a new pill. That’s why systems that include professional setup and follow-up-like those offered by Ennoble Care or through Medicare Advantage plans-have the best outcomes.


Chris porto
December 19, 2025 AT 07:08It’s funny how we treat pills like they’re magic beans. You take one, and suddenly you’re fixed. But nobody tells you the real cost-the mental load, the fear of messing up, the shame when you forget. I’ve seen my dad go from ‘I got this’ to ‘I don’t even know what I’m taking anymore.’ It’s not about gadgets. It’s about giving people space to be human.
Danielle Stewart
December 19, 2025 AT 10:30I’m a home health nurse, and this is exactly what we teach. The master list? Non-negotiable. The smart dispenser? Worth every penny if someone’s on 8+ meds. But the real win is when a family member actually sits down with them-not to ‘manage’ them, but to listen. That’s the glue holding it all together.
jessica .
December 20, 2025 AT 20:26THEY WANT YOU TO BUY THESE DEVICES SO THEY CAN TRACK YOU. YOU THINK THE PHARMACY CARES ABOUT YOUR HEALTH? NO. THEY WANT YOUR DATA. YOUR MEDS. YOUR BIOMETRICS. THEY’RE SELLING YOU TO BIG PHARMA. THE GOVT IS IN ON IT TOO. THAT ‘HOMEMEDS’ APP? IT’S A BACKDOOR. THEY’LL USE IT TO CUT YOUR BENEFITS LATER. DON’T FALL FOR IT.
Ryan van Leent
December 22, 2025 AT 05:51why do we even need all these pills in the first place? my grandpa lived to 92 on nothing but aspirin and beer. now everyone’s on 12 different things just to stay alive. doctors are just profit machines. they’d rather write scripts than fix the root cause. and now we’re supposed to buy $300 robots to take our meds? this is capitalism at its dumbest
Sajith Shams
December 23, 2025 AT 08:06Everyone talks about smart dispensers like they’re the solution. But have you ever tried using one if you don’t speak English? Or if you’re blind? Or if you live in a rural area with no Wi-Fi? This whole system is built for middle-class Americans with tech support. For the rest of us? We’re left guessing. And that’s not safety-that’s neglect dressed up as innovation.
Glen Arreglo
December 24, 2025 AT 06:08My mom’s from Mexico and she used to keep all her meds in a shoebox labeled with Sharpie. No app. No device. Just her and her calendar. She’s 84 and hasn’t had a mistake in 12 years. Technology helps-but it’s not sacred. The real tool is consistency, respect, and someone who cares enough to ask, ‘Did you take your pill today?’
shivam seo
December 25, 2025 AT 06:48U.S. healthcare is a joke. We spend billions on gadgets while people die because they can’t afford insulin. This article reads like a corporate ad for Hero Medical. Who funded this? Big Pharma? Medicare Advantage? The real solution is single-payer. Not a $300 robot that beeps when you forget your blood pressure pill.
benchidelle rivera
December 26, 2025 AT 09:00As someone who’s managed my mother’s regimen for seven years, I can say this: the printed list on the fridge saved her life twice. Once when she took her evening BP pill at breakfast. Again when the pharmacy gave her the wrong generic. No app could’ve caught that. No robot would’ve noticed she was trembling. Human eyes. Human hands. That’s what keeps people safe.
Isabel Rábago
December 26, 2025 AT 22:31It’s not about the system. It’s about control. People who are afraid of forgetting are afraid of losing autonomy. But the truth is, we’re all one bad day away from needing help. The smart dispenser isn’t a crutch-it’s a bridge. And if you think your memory is perfect, you haven’t been old long enough. I’ve watched my sister forget her insulin. Twice. She didn’t mean to. But forgetting isn’t weakness. It’s biology. And we owe it to each other to build systems that don’t punish that.
Anna Sedervay
December 27, 2025 AT 01:28While the article presents a superficially compelling narrative, one must interrogate the underlying epistemological assumptions: that technological augmentation is inherently benevolent, and that human cognition is a defect to be remediated by algorithmic surveillance. The notion that a $300 dispenser constitutes ‘safety’ is a neoliberal fantasy, obscuring the systemic failures of pharmaceutical overprescription and the erosion of intergenerational care. One wonders: who benefits from the commodification of vulnerability? The answer, as always, lies in the balance sheet-not the bedside.