Polycystic Ovary Syndrome (PCOS) affects about 1 in 10 women of childbearing age. It’s not just about irregular periods or acne-it’s a metabolic disorder rooted in insulin resistance. For many women, the real struggle isn’t just managing symptoms, but getting pregnant. That’s where metformin comes in. Originally developed as a diabetes drug, metformin has become a key player in treating PCOS-related infertility by targeting the root cause: insulin resistance.
How Metformin Works in PCOS
Metformin doesn’t trigger ovulation directly. Instead, it fixes the underlying problem-your body’s inability to use insulin properly. In women with PCOS, high insulin levels tell the ovaries to make more testosterone. That’s why many have irregular cycles, excess hair growth, or acne. Metformin lowers insulin by doing three things: it slows glucose absorption in the gut, reduces sugar production in the liver, and helps muscle cells absorb glucose more efficiently.
This isn’t just theory. A 2023 Cochrane review analyzed data from over 400 women and confirmed that metformin improves insulin sensitivity in PCOS patients. When insulin drops, testosterone drops too. And when testosterone drops, the ovaries start working normally again. The result? More regular ovulation.
Ovulation Rates: What the Data Shows
Studies show metformin increases ovulation rates significantly. One meta-analysis of 44 trials found women taking metformin were 2.5 times more likely to ovulate than those on placebo. In practical terms, that means about 60-70% of women on metformin start ovulating regularly within 3 to 6 months. That’s not as high as letrozole (which works in over 80% of cases), but it’s meaningful-especially for women who can’t or won’t take fertility drugs.
Here’s the catch: metformin works best when insulin resistance is the main driver. Women with PCOS who are lean but still insulin resistant often see the biggest improvement. In fact, some experts now argue that for non-obese women with PCOS, metformin should be the first choice-not clomiphene or letrozole.
Metformin vs. Other Fertility Treatments
For years, clomiphene citrate was the go-to drug for PCOS infertility. But newer evidence is shifting the landscape. A 2023 study of 72 women found that combining metformin with clomiphene led to higher ovulation rates than clomiphene alone. Even more telling: when women were resistant to clomiphene, adding metformin boosted their chances of pregnancy by nearly 40%.
Letrozole is now considered the most effective single-agent treatment for ovulation induction in PCOS. But metformin still has advantages. It’s cheaper-generic metformin costs $4 to $10 a month in the U.S., while letrozole can run $50 to $100. It also has fewer side effects than clomiphene, which can thin the uterine lining or cause mood swings.
And then there’s the IVF factor. If you’re going through in vitro fertilization, taking metformin before and during treatment cuts your risk of ovarian hyperstimulation syndrome (OHSS) by over 70%. That’s huge. OHSS can be dangerous, and preventing it means fewer hospital visits and less stress.

Real-World Results: Live Births and Pregnancy Rates
Does improved ovulation lead to more babies? The answer is yes-but with nuance. The same Cochrane review that found metformin improved ovulation also showed it increased live birth rates compared to placebo. The odds ratio was 1.59, meaning women on metformin had a 59% higher chance of having a baby. That translates to a rise from about 19% to between 19% and 37% live birth rates.
But here’s where it gets tricky. Some clinics report that metformin alone doesn’t dramatically improve pregnancy rates over placebo. Why? Because ovulation doesn’t always mean conception. You still need timing, sperm quality, and healthy fallopian tubes. That’s why most doctors recommend combining metformin with other strategies-like tracking ovulation with progesterone tests or having sex every 2 to 3 days during your fertile window.
How to Take Metformin for PCOS
Most doctors start at 500mg once a day with dinner. After a week or two, they increase to 500mg twice daily. The goal is usually 1,500mg to 2,000mg per day. It takes time. Don’t expect results in 2 weeks. Most women notice regular periods after 2 to 3 months. Ovulation usually kicks in by month 4.
There are two forms: immediate-release and extended-release (XR). The XR version is gentler on the stomach. About 20-30% of people get nausea, diarrhea, or bloating at first. These side effects fade in most cases within 4 to 6 weeks. If they don’t, switching to XR often helps.
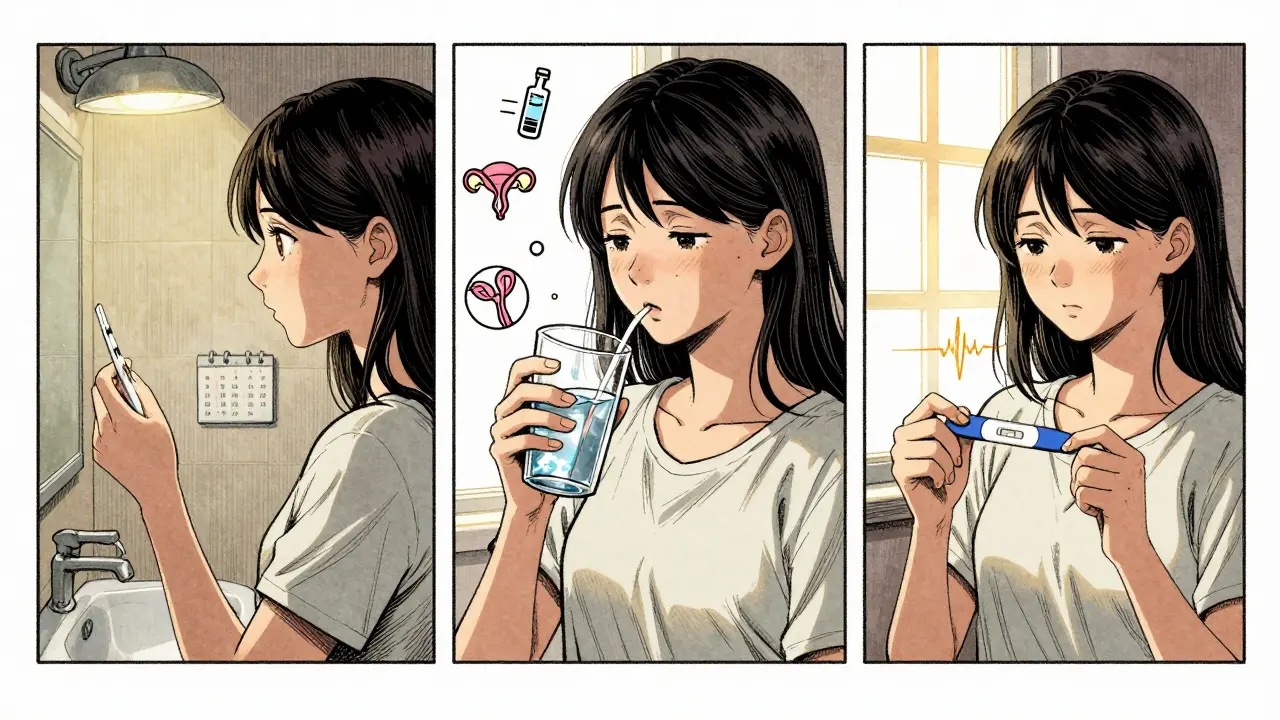
Before starting, you need a negative pregnancy test. Metformin is safe during pregnancy (Category B), and some studies suggest continuing it through the first trimester may improve pregnancy outcomes. But always check with your doctor. Some OB-GYNs prefer to stop it once you’re pregnant; others keep it going to reduce miscarriage risk.
Beyond Fertility: Other Benefits
Metformin isn’t just for trying to conceive. Many women take it long-term to manage PCOS symptoms. It can reduce facial hair, clear up acne, and even help with weight loss-especially when paired with diet and exercise. It’s also the only medication proven to lower long-term risks like type 2 diabetes and heart disease in PCOS patients.
A 2017 study called REPOSE followed women with PCOS for years and found metformin users had a lower chance of developing diabetes. That’s huge. PCOS isn’t just a reproductive issue-it’s a lifelong metabolic condition. Metformin addresses both.
Who Benefits Most?
Not every woman with PCOS needs metformin. The best candidates are those with:
- Insulin resistance (confirmed by blood tests like fasting insulin or HOMA-IR)
- Irregular or absent periods
- Normal or low body weight (lean PCOS)
- High androgen levels (testosterone, DHEA-S)
- Trying to conceive without success
Women with severe obesity may still benefit, but weight loss and lifestyle changes are usually tried first. Metformin works best as a partner to diet, not a replacement.
What to Expect Long-Term
Metformin isn’t a cure. It’s a tool. Some women take it for months; others stay on it for years. If you stop, insulin resistance and irregular cycles often return. But if you stick with it, many report more than just fertility improvements-they feel better overall. More energy. Fewer cravings. Clearer skin. Better mood.
One woman from Manchester shared on a patient forum: "I started metformin at 28. I’d been trying for 2 years. No one told me to test my insulin. After 3 months, my period came back. After 6, I got pregnant. I’m still on it. My doctor says it’s protecting me from diabetes. I’m not taking chances."
That’s the story behind the data. Metformin isn’t flashy. It doesn’t promise quick results. But for the right woman, it changes everything.
Can metformin help me get pregnant if I have PCOS?
Yes, metformin can improve your chances of getting pregnant if you have PCOS and insulin resistance. It helps restore regular ovulation by lowering insulin and testosterone levels. Studies show it doubles the odds of ovulation compared to no treatment. For best results, combine it with timed intercourse or other fertility treatments like letrozole.
How long does it take for metformin to work for PCOS?
Most women start seeing changes in their menstrual cycle after 2 to 3 months. Ovulation usually returns between 3 and 6 months. For fertility purposes, doctors typically recommend taking metformin for at least 3 months before trying to conceive. Some women need up to 6 months to see full effects.
Is metformin better than clomiphene for PCOS infertility?
It depends. Clomiphene is more effective at triggering ovulation on its own. But metformin addresses the root cause-insulin resistance-and has fewer side effects. For women with lean PCOS or insulin resistance, metformin may be just as effective. Many doctors now use them together: metformin to improve insulin sensitivity, clomiphene to boost ovulation. This combo often works better than either drug alone.
Does metformin cause weight loss in PCOS?
Metformin can help with modest weight loss-usually 2 to 5% of body weight-especially when combined with diet and exercise. It reduces appetite and cravings by stabilizing blood sugar. It’s not a weight-loss drug, but for women with PCOS, even a small drop in weight improves insulin sensitivity and ovulation.
Can I take metformin while pregnant?
Yes, metformin is considered safe during pregnancy (Category B). Some studies suggest continuing it in the first trimester may reduce miscarriage risk and improve outcomes in women with PCOS. However, many OB-GYNs stop it once pregnancy is confirmed. Always discuss this with your doctor-it’s a personal decision based on your health history.
What are the side effects of metformin for PCOS?
The most common side effects are stomach-related: nausea, diarrhea, bloating, or gas. These happen in about 20-30% of users, especially at the start. They usually fade within 2 to 4 weeks. Switching to the extended-release (XR) form can reduce these side effects. Rarely, metformin can cause vitamin B12 deficiency over time, so periodic blood tests are recommended.
Do I need to take metformin forever if I have PCOS?
No, you don’t need to take it forever. If you get pregnant and your periods return, your doctor may suggest stopping it. But if you still have insulin resistance, irregular cycles, or metabolic risks, long-term use may be recommended. Many women with PCOS stay on metformin for years-not for fertility, but to protect against diabetes and heart disease.


Mark Harris
February 7, 2026 AT 05:42Marcus Jackson
February 8, 2026 AT 13:21Natasha Bhala
February 9, 2026 AT 08:49Ashley Hutchins
February 10, 2026 AT 18:39Paula Sa
February 12, 2026 AT 08:09Ritu Singh
February 13, 2026 AT 05:58Catherine Wybourne
February 13, 2026 AT 11:35Niel Amstrong Stein
February 15, 2026 AT 00:17Mary Carroll Allen
February 16, 2026 AT 06:01Mark Harris
February 16, 2026 AT 20:08Tola Adedipe
February 17, 2026 AT 23:03Mayank Dobhal
February 18, 2026 AT 00:02