NSAID Gastrointestinal Risk Calculator
NSAID Safety Assessment
This tool estimates your risk of gastrointestinal bleeding from NSAID use based on key risk factors. The American College of Gastroenterology states that having two or more risk factors increases your risk significantly. Know your risk before taking NSAIDs.
Enter your risk factors and click "Calculate My Risk" to see your assessment
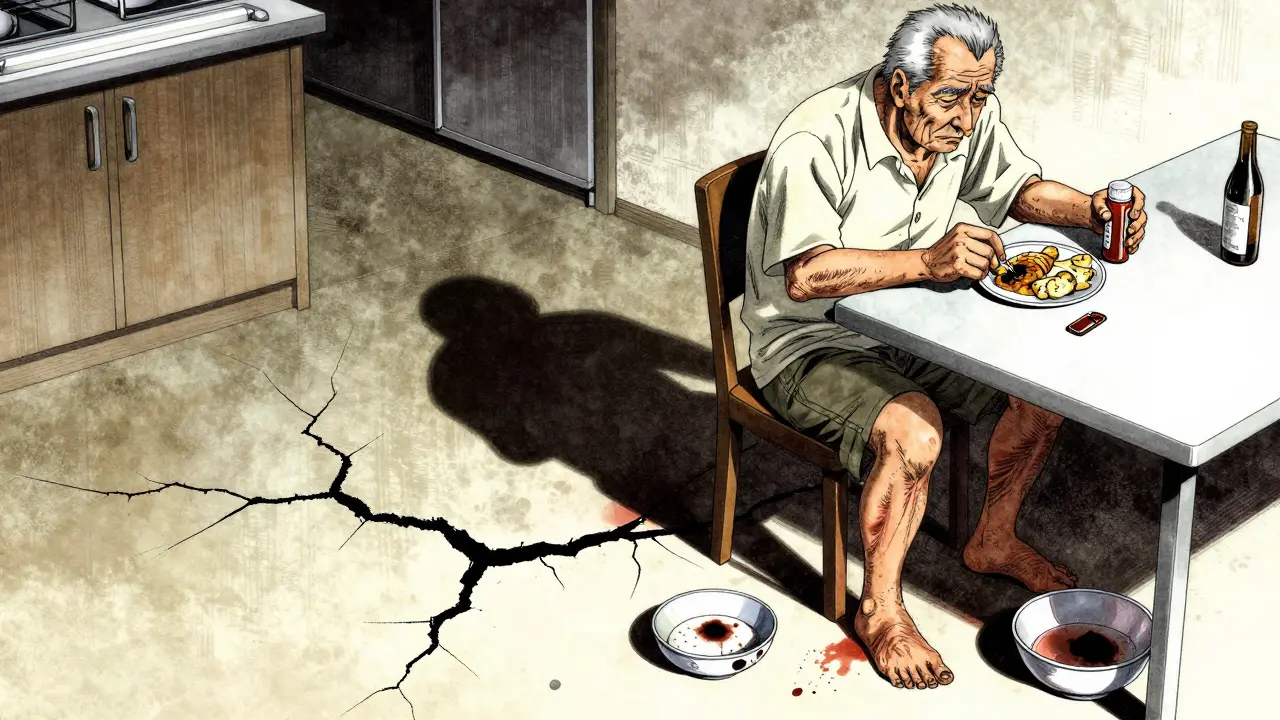
Every year, millions of people reach for ibuprofen, naproxen, or diclofenac to ease aching joints, headaches, or back pain. These are NSAIDs-non-steroidal anti-inflammatory drugs-and they work. But for many, they also silently damage the stomach and intestines. What starts as mild indigestion can turn into a life-threatening bleed without warning. If you or someone you know takes NSAIDs regularly, you need to know the real risk: NSAIDs are one of the leading causes of gastrointestinal bleeding, especially in older adults.
How NSAIDs Cause Ulcers and Bleeding
NSAIDs don’t just block pain signals-they shut down protective mechanisms in your gut. They inhibit COX-1 enzymes, which are responsible for producing prostaglandins that keep the stomach lining healthy. These prostaglandins help maintain mucus and blood flow to the stomach and duodenum. Without them, the lining becomes vulnerable. Even a short course of NSAIDs can cause tiny erosions. Over time, these turn into ulcers. And ulcers don’t always hurt. Many people don’t feel anything until they start vomiting blood, passing black tarry stools, or suddenly feel dizzy from internal bleeding.
It’s not just about big, obvious ulcers. Studies show that up to 86% of people with lower GI bleeding who took NSAIDs didn’t even have a classic peptic ulcer. The damage can happen anywhere in the digestive tract-from the stomach down to the small intestine. The Cleveland Clinic found that NSAID-related lesions range from superficial scrapes (Grade 1) to deep ulcers with visible blood vessels (Grade 4). The higher the grade, the more likely it is to bleed.
Who’s at the Highest Risk?
Not everyone who takes NSAIDs will bleed. But some people are far more vulnerable. The biggest risk factors are well-documented:
- Age over 65-risk doubles with each decade
- History of peptic ulcer or prior GI bleed
- Taking blood thinners like warfarin or aspirin
- Using corticosteroids (like prednisone)
- Taking more than one NSAID at a time
- High doses-over 1,200 mg of ibuprofen daily
- Having other serious illnesses like heart failure or kidney disease
If you have two or more of these, your risk isn’t just elevated-it’s dangerous. A 2017 Cochrane review showed that people with multiple risk factors are up to six times more likely to suffer a serious bleed than those with none. And here’s the scary part: many don’t know they’re at risk. A 2022 survey on HealthUnlocked found that 63% of NSAID users had GI symptoms like bloating, nausea, or dark stools, but only 37% told their doctor.
NSAID Types: Not All Are Equal
There’s a big difference between traditional NSAIDs and newer ones. Non-selective NSAIDs like ibuprofen, naproxen, and diclofenac block both COX-1 and COX-2. That’s why they’re effective for pain but also hard on the stomach. Selective COX-2 inhibitors-like celecoxib (Celebrex)-were designed to spare COX-1. The 2000 Lancet study showed celecoxib had half the rate of serious ulcers compared to ibuprofen.
But there’s a trade-off. The 2004 APPROVe trial found that rofecoxib (Vioxx) doubled the risk of heart attack. That drug was pulled from the market. Celecoxib still carries a cardiovascular warning, but it’s considered safer than older COX-2 drugs. For people with high GI risk but low heart risk, celecoxib may be a better choice. But it’s not risk-free.

Protecting Your Gut: What Actually Works
If you need NSAIDs and have risk factors, you need protection. And not just any protection-evidence-backed protection.
Proton pump inhibitors (PPIs) are the gold standard. Omeprazole, esomeprazole, pantoprazole-these drugs reduce stomach acid so much that ulcers can heal and new ones are prevented. A 2017 Cochrane review of over 13,000 patients showed PPIs cut NSAID-related ulcer complications by 75%. That’s not a small benefit-it’s life-saving. The American College of Gastroenterology recommends PPIs for anyone with a prior bleed or two or more risk factors.
Another option is misoprostol, a synthetic prostaglandin. It’s effective-cutting ulcer risk by 50-75%-but it’s tough to tolerate. Up to 20% of people get diarrhea. Others have cramps or nausea. Because of this, it’s rarely used unless someone can’t take a PPI.
Then there’s the new combo drug: naproxen/esomeprazole (Vimovo). Approved by the FDA in 2023, it combines the pain relief of naproxen with the gut protection of esomeprazole in one pill. In the PRECISION-2 trial, only 7.3% of people on Vimovo developed ulcers compared to 25.6% on naproxen alone. It’s not cheap, but for high-risk patients, it’s a game-changer.
The Hidden Cost: Bleeding Isn’t Always Obvious
Most people think of GI bleeding as vomiting blood or passing black stool. But that’s the worst-case scenario. Far more common is occult bleeding-slow, silent blood loss that doesn’t cause pain or visible signs. This leads to iron deficiency anemia. People feel tired, short of breath, pale. They go to the doctor thinking they’re just “getting older.” But the real cause? Years of daily NSAID use.
One Reddit user, u/ElderCareHelper, shared how their 78-year-old mother needed three blood transfusions after months of unexplained fatigue. Her hemoglobin had dropped to 6.8 g/dL (normal is 12-16). No abdominal pain. No vomiting. Just a slow, silent bleed from NSAID-damaged intestines. She’d been taking ibuprofen daily for arthritis for over a decade.
According to a 2019 Pharmacoepidemiology study, NSAIDs cause about 107,000 hospitalizations and 16,500 deaths each year in the U.S. alone. That’s more than traffic accidents in some years. And it’s preventable.
What Should You Do?
Here’s what works in real life:
- If you’re over 65, have a history of ulcers, or take blood thinners-don’t start NSAIDs without talking to your doctor.
- If you’re already taking NSAIDs, ask: “Am I at risk? Do I need a PPI?”
- Use the lowest dose for the shortest time possible. Even 5-7 days of high-dose ibuprofen can trigger bleeding in vulnerable people.
- Don’t assume OTC means safe. Over-the-counter NSAIDs are often taken at double the recommended dose. A 2021 review found 26% of users exceed daily limits.
- Get a blood test if you’re tired, pale, or short of breath. Check your iron and hemoglobin. Anemia can be the only sign of internal bleeding.
- If you’re on long-term NSAIDs, ask about Vimovo or celecoxib + PPI. It’s not about avoiding pain relief-it’s about avoiding hospitalization.
There’s no magic pill that makes NSAIDs safe. But there are clear, proven steps to reduce the risk. Ignoring it isn’t bravery-it’s dangerous.

What About Alternatives?
If NSAIDs are too risky, what else works? For arthritis and chronic pain:
- Physical therapy and exercise-proven to reduce pain as effectively as NSAIDs in many cases
- Topical diclofenac gel-less absorbed into the bloodstream, so lower GI risk
- Acetaminophen (paracetamol)-no GI bleeding risk, but doesn’t reduce inflammation
- Non-drug options: heat therapy, weight loss, braces, or joint injections
For acute pain like a sprain or headache, NSAIDs are fine for a few days. But if you’re using them every day for months or years, you’re playing with fire. The body doesn’t adapt to the damage-it just accumulates it.
Future Hope: New Drugs on the Horizon
Scientists are working on safer NSAIDs. One promising class is CINODs-COX-inhibiting nitric oxide donors. Naproxcinod, tested in the 2021 NAPROX-2 trial, cut endoscopic ulcers by 50% compared to naproxen. And unlike COX-2 inhibitors, it didn’t raise blood pressure or heart risk. It’s still in phase III trials, but it could be the first NSAID that doesn’t wreck the gut.
Until then, the best tool we have is awareness. Knowing your risk. Asking the right questions. Using protection when needed.
Can I take ibuprofen if I’ve had a stomach ulcer before?
No, not without serious precautions. If you’ve had a prior ulcer or bleed, taking NSAIDs again carries a very high risk of another bleed-up to 10 times higher than someone without a history. The American College of Gastroenterology recommends COX-2 inhibitors like celecoxib combined with a proton pump inhibitor (PPI) for these patients. Never restart NSAIDs without discussing it with your doctor.
Do all NSAIDs cause the same level of bleeding risk?
No. Non-selective NSAIDs like naproxen and diclofenac carry the highest GI risk. Ibuprofen is slightly lower but still dangerous at high doses or with other risk factors. Selective COX-2 inhibitors like celecoxib have about half the risk of ulcers and bleeding compared to traditional NSAIDs. However, they come with their own risks, especially for the heart. The choice depends on your individual health profile.
Is it safe to take OTC NSAIDs every day?
Not for most people. Over-the-counter NSAIDs are meant for short-term use-no more than 10 days without medical advice. Daily use, even at low doses, increases your risk of ulcers and bleeding over time. Many people don’t realize they’re at risk because they don’t feel symptoms until it’s too late. If you need daily pain relief, talk to your doctor about safer alternatives.
Can PPIs completely prevent NSAID-induced bleeding?
No, but they reduce the risk by about 75%. PPIs are highly effective at preventing ulcers and bleeding, but they’re not 100% foolproof. People on blood thinners or with multiple risk factors still have a small chance of bleeding even while taking a PPI. That’s why doctors recommend combining PPIs with other strategies-like using the lowest NSAID dose possible or switching to a COX-2 inhibitor.
What are the signs of NSAID-related bleeding I should watch for?
Watch for black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, sudden dizziness or weakness, or unexplained fatigue and pale skin. These can signal major bleeding. But sometimes the only sign is iron deficiency anemia-low energy, shortness of breath, or rapid heartbeat. If you’ve been taking NSAIDs regularly and feel unusually tired, get a blood test. Silent bleeding is common and deadly.
Is naproxen/esomeprazole (Vimovo) better than taking naproxen and a PPI separately?
Yes, for people who need both. Vimovo combines the two in one pill, so you’re less likely to forget the PPI. Studies show it reduces ulcer complications by more than two-thirds compared to naproxen alone. It’s especially useful for high-risk patients who need long-term NSAID therapy. The downside is cost-it’s more expensive than generic naproxen and omeprazole separately. But for many, the convenience and proven safety make it worth it.
Final Takeaway
NSAIDs are powerful tools. But they’re not harmless. For millions, they’re a daily necessity. For others, they’re a ticking time bomb. The difference is awareness. Know your risk. Ask your doctor. Use protection. Don’t wait for a bleed to happen before you act. Pain management shouldn’t cost you your health.

Marie Mee
December 17, 2025 AT 04:24My neighbor took ibuprofen for years and ended up in the ER with a hole in her stomach
They don't tell you this stuff because they make money off the surgeries
Naomi Lopez
December 17, 2025 AT 21:49Linda Caldwell
December 19, 2025 AT 05:59Don't let fear stop you from living-just talk to your doc and get smart about it
Anna Giakoumakatou
December 19, 2025 AT 14:07CAROL MUTISO
December 19, 2025 AT 21:04Erik J
December 21, 2025 AT 20:03BETH VON KAUFFMANN
December 22, 2025 AT 18:07Martin Spedding
December 23, 2025 AT 17:57Big Pharma owns the FDA
They’re all in on the pain pill racket
Raven C
December 23, 2025 AT 22:29Jessica Salgado
December 24, 2025 AT 16:33Peter Ronai
December 24, 2025 AT 18:25Steven Lavoie
December 25, 2025 AT 08:44Michael Whitaker
December 26, 2025 AT 08:08Brooks Beveridge
December 27, 2025 AT 04:14Switching to Vimovo changed my life
My back still hurts sometimes-but now I'm not scared to wake up
Keep going, you got this!