Medication Risk Calculator for Dizziness on Standing
This tool helps you assess your risk of orthostatic hypotension based on medications you're taking. Based on your inputs, it calculates your relative risk and provides personalized recommendations.
Your Risk Assessment
- Each high-risk medication category adds 20-40% risk
- 5+ medications increases risk by 5x
- Age and other conditions also affect risk
Standing up too fast and feeling like the room is spinning? That’s not just being clumsy. It could be orthostatic hypotension - a sudden drop in blood pressure when you rise from sitting or lying down. For many people, especially those on multiple medications, this isn’t rare. It’s a common, often overlooked side effect that can lead to falls, injuries, and even hospital visits.
What Exactly Is Orthostatic Hypotension?
Orthostatic hypotension, also called postural hypotension, happens when your blood pressure drops more than 20 mm Hg systolic or 10 mm Hg diastolic within three minutes of standing. Your body normally adjusts quickly when you stand - blood vessels tighten, your heart beats faster, and blood keeps flowing to your brain. But when that system fails, you get dizzy, lightheaded, or worse - you faint. This isn’t just about feeling a little woozy. Studies show people with this condition have a 15-30% higher chance of falling. Over 10 years, their risk of death increases by 24-32%. The good news? When it’s caused by medications, it’s often reversible.Which Medications Cause Dizziness on Standing?
Not all drugs affect blood pressure the same way. Some interfere with your body’s natural ability to regulate blood flow when you stand. Here are the biggest culprits:- Antipsychotics - Drugs like clozapine, quetiapine, and chlorpromazine block receptors that help keep blood pressure stable. Up to 40% of people taking these at higher doses experience orthostatic hypotension.
- Alpha-blockers - Used for high blood pressure or prostate issues, drugs like doxazosin and terazosin relax blood vessels too much. Their odds of causing OH are nearly 3 times higher than other blood pressure meds.
- Diuretics - Water pills like hydrochlorothiazide reduce blood volume. Less fluid means less pressure to push blood upward when you stand. Risk increases 1.9 times.
- Tricyclic antidepressants - Amitriptyline and nortriptyline disrupt nerve signals that control blood pressure. They carry a 3.2 times higher risk of OH.
- Opioids - Morphine, oxycodone, and hydrocodone can cause dizziness in 15-25% of older adults. The risk jumps 2.3 times if taken with alcohol or benzodiazepines.
- Levodopa - Used for Parkinson’s, this drug affects the autonomic nervous system. Between 30-50% of patients on levodopa develop OH.
It’s not just the drug - it’s the combo. Someone on five or more medications has over five times the risk of OH compared to someone on one or two. That’s why polypharmacy is such a silent danger.
Why Do Older Adults Get This More Often?
Age isn’t just a number here. As we get older, our blood vessels stiffen, our heart rate response slows, and our baroreceptors - the sensors that detect blood pressure changes - don’t work as well. Add medications into the mix, and the system breaks down faster. People over 70 are 3.2 times more likely to develop drug-induced orthostatic hypotension than younger adults. And if they’re already dealing with diabetes, Parkinson’s, or heart failure? The risk skyrockets. Many older patients are on multiple drugs for these conditions - each one adding another layer of risk.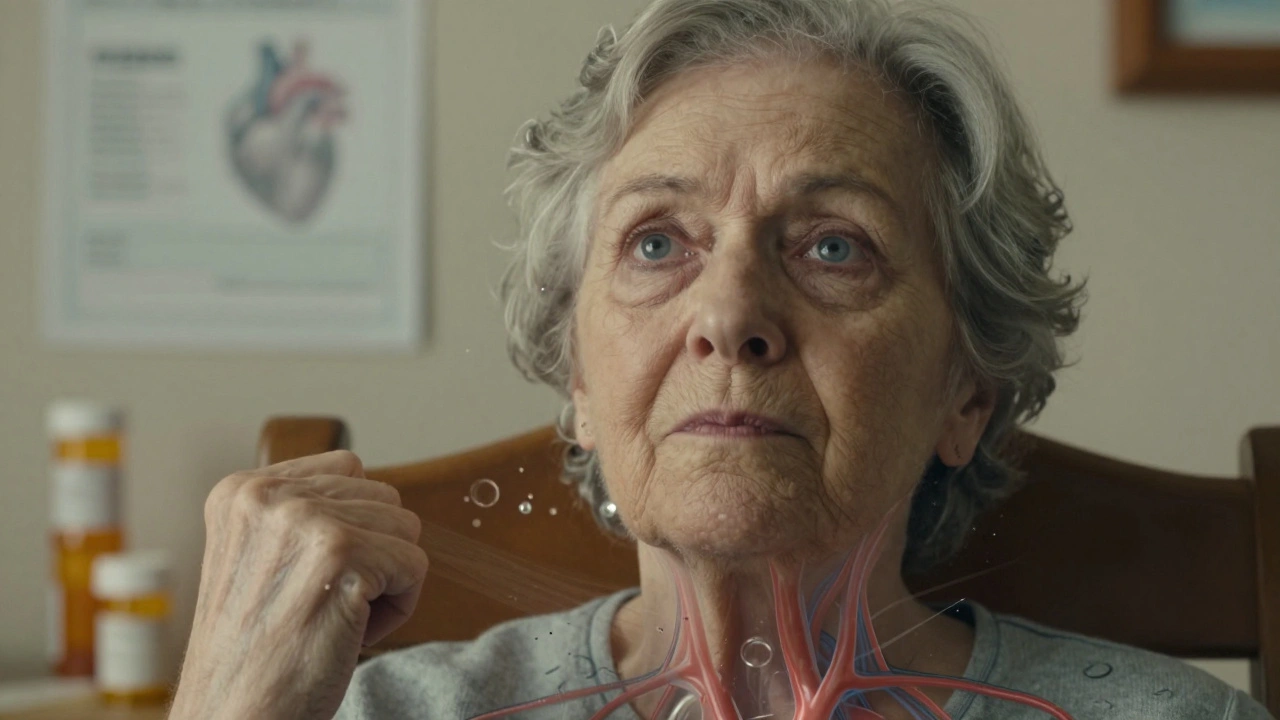
How Do You Know It’s Medication-Related?
Not every dizzy spell is OH. But if you notice dizziness, blurred vision, or weakness only when standing - and it goes away when you sit or lie back down - it’s a strong clue. Symptoms usually hit within 1-3 minutes of standing. Some people feel fine sitting, then suddenly feel like they’re going to pass out when they get up to get a glass of water. Doctors diagnose it by measuring blood pressure. You lie down for five minutes. Then you stand up. Blood pressure is checked at 1, 2, and 3 minutes after standing. If it drops more than 20/10 mm Hg and you have symptoms, that’s a diagnosis. Here’s the catch: up to 40% of people with OH don’t even feel symptoms. That’s why screening matters - especially in older adults on multiple meds. A simple check during a routine visit can catch it before a fall happens.What Can You Do About It?
The best treatment? Often, it’s not another drug. It’s adjusting the ones you’re already taking.- Review your meds - Talk to your doctor or pharmacist. Ask: “Could any of these be causing my dizziness?” Don’t stop anything on your own, but do bring a full list - including supplements and over-the-counter drugs.
- Lower the dose - Sometimes, reducing the amount of a medication helps. For example, lowering quetiapine from 100 mg to 50 mg can cut OH symptoms without losing its benefit.
- Switch medications - If you’re on an older antipsychotic like clozapine, newer ones like ziprasidone carry much lower OH risk. For blood pressure, switching from an alpha-blocker to an ACE inhibitor might help.
- Time your doses - Take blood pressure-lowering meds at night if possible. That way, the peak effect isn’t when you’re getting up in the morning.
Non-drug fixes work too:
- Stand up slowly - Sit on the edge of the bed for a minute before standing. Pause before walking.
- Drink more water - Aim for 2-2.5 liters a day. Dehydration makes OH worse.
- Wear compression stockings - These help push blood back up from your legs. They’re simple, cheap, and effective.
- Elevate the head of your bed - Raising the head by 6-10 inches helps your body retain fluid overnight and reduces morning drops in BP.
- Avoid heat and alcohol - Hot showers, saunas, and alcohol dilate blood vessels and make dizziness worse.
Studies show 65-80% of people feel better within 1-2 weeks after adjusting their meds. One patient, 78, had recurrent falls. After stopping hydrochlorothiazide, her symptoms vanished in 72 hours.
When Medication Is Still Needed
Sometimes, you can’t just stop a drug. If you have Parkinson’s and need levodopa, or severe depression requiring an antidepressant, the risk must be managed - not eliminated. In those cases, doctors may add a medication like midodrine - a drug that tightens blood vessels. It’s taken three times a day and reduces dizziness in 65% of patients. But it’s not a first-line fix. It’s used only when lifestyle changes and medication adjustments aren’t enough.
What Happens If You Ignore It?
Ignoring dizziness on standing isn’t harmless. Falls are the leading cause of injury-related deaths in people over 65. A single fall can lead to hip fractures, brain bleeds, or long-term disability. And OH doesn’t just increase fall risk - it’s linked to cognitive decline and higher death rates over time. Many patients don’t connect their dizziness to their meds. In one Mayo Clinic study, 55% of people had symptoms for over two months before anyone realized it was drug-related. By then, they’d already fallen once or twice.How to Talk to Your Doctor
Don’t wait for a fall. If you’re on any of the high-risk medications listed above - especially if you’re over 65 - ask these questions:- “Could any of my medications be making me dizzy when I stand?”
- “Can we review all my meds together - including supplements?”
- “Is there a lower-risk alternative for this drug?”
- “Should I get my blood pressure checked when I stand up?”
Most doctors aren’t trained to screen for OH routinely. But if you bring up the issue, they’re more likely to check. The American Geriatrics Society recommends all older adults on multiple meds be screened for orthostatic hypotension.
The Bigger Picture
Medication-induced orthostatic hypotension isn’t rare. It’s preventable. And it’s costing the U.S. healthcare system over $9 billion a year in fall-related care - much of it tied to drugs that could be adjusted. Newer medications are being developed to avoid this side effect entirely. But for now, the best tool we have is awareness - and a willingness to question whether a drug is doing more harm than good.If you’re feeling dizzy when you stand up - don’t brush it off. It’s not just aging. It’s a signal. Your body is telling you something’s off. And with the right changes, you can stand up without fear.
Can orthostatic hypotension go away on its own?
Yes - if it’s caused by medications. In 70-85% of cases, symptoms improve or disappear after adjusting or stopping the drug. But if it’s caused by nerve damage from Parkinson’s or diabetes, it’s less likely to resolve without treatment. The key is identifying the cause.
Is orthostatic hypotension dangerous?
It can be. While dizziness itself isn’t life-threatening, the risk of falling is serious. Falls lead to fractures, head injuries, and hospitalizations. People with OH also have a 24-32% higher long-term risk of death, partly because it’s a sign of underlying problems with blood pressure control.
Which is worse: diuretics or alpha-blockers for causing dizziness?
Alpha-blockers carry a higher risk - about 2.8 times more likely to cause orthostatic hypotension than other blood pressure drugs. Diuretics are still risky (1.9 times higher), especially if you’re dehydrated. But alpha-blockers like doxazosin or terazosin are more directly linked to sudden drops in blood pressure upon standing.
Should I stop my medication if I feel dizzy?
No. Never stop a medication without talking to your doctor. Some drugs, like those for heart disease or depression, can be dangerous to stop suddenly. Instead, write down when and how often you feel dizzy, then bring it to your next appointment. Your doctor can help you adjust safely.
Can I prevent orthostatic hypotension before it starts?
Yes. If you’re starting a new medication known to cause OH - like an alpha-blocker or antipsychotic - ask your doctor to check your blood pressure standing up after your first dose. Stay hydrated, avoid alcohol, and stand up slowly from the start. Prevention is easier than fixing it after a fall.

Michael Robinson
December 10, 2025 AT 01:14It’s not just about the meds. It’s about how we treat aging like a bug to be fixed instead of a process to understand. We slap on pills like stickers and wonder why people fall. Maybe the real problem isn’t the drugs-it’s that we’ve forgotten how to listen to our bodies.
Iris Carmen
December 10, 2025 AT 15:11ive been dizzy since i started my bp med and thought it was just me being old. guess i’m not crazy lol
Andrea DeWinter
December 11, 2025 AT 15:07For anyone reading this and feeling overwhelmed-start with the basics. Write down every pill, supplement, and even that herbal tea you take. Bring it to your doc. Don’t assume they know everything you’re on. I helped my mom cut three meds that were making her dizzy. She hasn’t fallen in a year. Simple. Not glamorous. Life-changing.
Raja Herbal
December 12, 2025 AT 07:19So in america you just pop pills for everything and then wonder why you feel like a zombie standing up. here in india we just sit down and wait for the dizziness to pass. sometimes the medicine is the problem, not the cure.
Sarah Gray
December 12, 2025 AT 08:44Let’s be honest-this isn’t even news. Anyone with half a brain and access to PubMed knows that polypharmacy in the elderly is a disaster waiting to happen. The fact that this is still being treated as some novel insight is a indictment of modern medicine’s obsession with prescribing over thinking. The real scandal? Doctors don’t even check orthostatic BP routinely. They’re too busy checking off boxes to actually care if you live or fall.
Rich Paul
December 14, 2025 AT 06:08bro just get compression socks and chug water like its your job. also stop taking that 50mg quetiapine at 7am. take it at 9pm and boom-no more faceplanting into the cereal aisle. i’m not a doctor but i play one on reddit and my aunt survived 3 falls after i told her this. also avoid hot showers. like bro, it’s not 2003 anymore, stop acting like a sauna is self care.
Kathy Haverly
December 14, 2025 AT 22:41Oh wow, another ‘meds are bad’ post. Let me guess-you’re one of those people who thinks if you just ‘eat more kale’ and ‘breathe deeply’ you won’t need antidepressants? Newsflash: some people have real illnesses. Levodopa isn’t optional. If you can’t tolerate side effects, maybe you shouldn’t have Parkinson’s. And don’t get me started on ‘switching meds’-you think it’s that easy? Half the time the alternatives are worse, cost more, or don’t work at all. This isn’t a DIY fix-it guide. It’s a chronic condition with trade-offs. Stop oversimplifying.
George Taylor
December 15, 2025 AT 17:27...and yet... the article doesn’t mention... that... the... American Geriatrics Society... recommends... screening... for... all... patients... on... three... or... more... medications... which... is... not... happening... in... 90%... of... clinics... because... of... time... constraints... and... reimbursement... issues... and... also... because... doctors... are... tired... and... overworked... and... honestly... most... patients... don’t... even... mention... dizziness... because... they... think... it’s... just... aging... and... they... don’t... want... to... be... a... burden... so... we... keep... prescribing... and... keep... watching... people... fall... and... nobody... does... anything... because... it’s... too... complicated... and... nobody... wants... to... talk... about... it...