REM Sleep Calculator
REM sleep is a critical stage of rest that helps regulate pain perception. Based on your total sleep duration, we can estimate your ideal REM sleep time based on clinical guidelines (20-25% of total sleep).
Your Ideal REM Sleep Range
Enter your total sleep time to see results
Why this matters for chronic pain: Studies show that maintaining 20-25% REM sleep can help regulate neurotransmitters, reduce inflammation, and lower pain sensitivity. Less REM sleep is associated with higher pain scores in chronic conditions like fibromyalgia and arthritis.
Quick Takeaways
- REM sleep is a deep, dreaming stage that influences pain perception.
- Reduced REM time is linked to higher pain intensity in chronic conditions.
- Key mechanisms include neurotransmitter balance, hormone swings, and inflammation.
- Improving sleep hygiene, managing stress, and using light therapy can boost REM.
- If pain spikes despite better sleep, a specialist assessment is essential.
Understanding why a restless night can make aches flare up starts with two basics: Rapid Eye Movement (REM) sleep is a stage of sleep marked by vivid dreaming, rapid eye movements, and heightened brain activity and chronic pain is a persistent pain lasting longer than three months that often resists standard treatments. This article walks through what science says about their link and gives practical steps to turn sleepless nights into a pain‑relief ally.
What Exactly Is REM Sleep?
Sleep isn’t a single block; it cycles through stages. The sleep cycle comprises light sleep, deep (slow‑wave) sleep, and REM sleep, repeating every 90-120 minutes throughout the night. During REM, the brain’s electrical activity mirrors wakefulness, muscles are paralyzed, and the heart rate can jump. This stage is crucial for emotional processing, memory consolidation, and, as emerging research shows, pain modulation.
Chronic Pain 101
Conditions like fibromyalgia, osteoarthritis, and neuropathic pain fall under the chronic pain umbrella term for long‑lasting discomfort that often involves both peripheral and central nervous system changes. It isn’t just a signal from a hurt tissue; the nervous system rewires, lowering the pain threshold the point at which a stimulus becomes painful and amplifying signals.
How Sleep Architecture Influences Pain
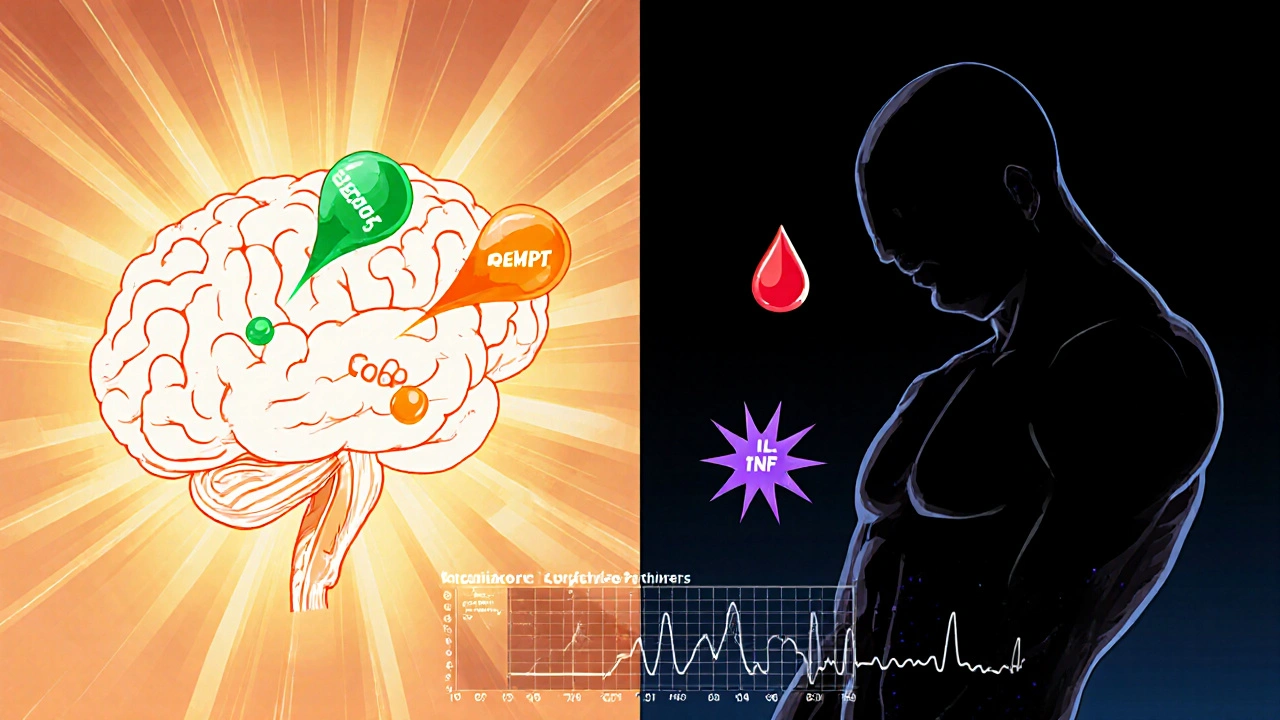
When REM time drops, the body misses a nightly “reset”. Studies using polysomnography an overnight test that records brain waves, eye movements, heart rhythm, and breathing have found that participants with less REM report higher pain scores the next day. The reasons are threefold:
- Neurotransmitter imbalance: REM boosts serotonin and dopamine, both of which dampen pain signals. A deficiency can leave the nervous system in a hyper‑excitable state.
- Hormonal swings: melatonin a hormone that regulates sleep‑wake cycles peaks during the night, while cortisol the stress hormone that can increase inflammation falls. Disrupted REM skews this balance, prompting inflammation.
- Inflammatory cytokines: During REM, levels of interleukin‑6 (IL‑6) a cytokine that can heighten pain sensitivity and tumor necrosis factor‑alpha (TNF‑α) another pain‑promoting cytokine dip. Skipping REM keeps these molecules elevated.
Scientific Evidence Linking REM and Chronic Pain
One 2023 longitudinal study of 312 fibromyalgia patients used nightly actigraphy to track sleep stages. Participants with a nightly REM proportion under 20% experienced a 1.8‑point rise on the Visual Analogue Scale (VAS) for pain over six months, compared with a stable VAS in those maintaining 25%+REM. Another 2022 randomized trial gave veterans with PTSD‑related chronic pain a REM‑enhancing protocol (bright‑light exposure in the evening plus melatonin 0.5mg). After eight weeks, REM duration grew by 15 minutes on average, and reported pain fell by 22%.
These numbers aren’t magic bullets, but they consistently show that when REM recovers, pain often eases.
The Core Biological Pathways
Neurotransmitters
During REM, the brain releases higher levels of serotonin a neurotransmitter that modulates mood and pain perception and dopamine. Both act on spinal cord receptors to inhibit nociceptive (pain‑carrying) signals. Chronic pain patients often show reduced serotonergic activity, making REM a natural counterbalance.
Hormones
Melatonin produced by the pineal gland, peaks at night and supports REM onset also has analgesic properties. Supplementing melatonin in low‑dose form (0.3-0.5mg) has been shown to increase REM proportion and modestly lower pain scores in migraine sufferers.
Conversely, cortisol rises in response to stress and can exacerbate inflammation typically drops during deep REM. When REM is truncated, cortisol’s nighttime dip flattens, leaving the body in a low‑grade stress state.
Inflammatory Cytokines
REM appears to act as a nightly anti‑inflammatory checkpoint. Researchers measuring blood samples before and after REM‑rich sleep found a 30% reduction in IL‑6 and TNF‑α. Elevated cytokines are a hallmark of conditions like rheumatoid arthritis, suggesting that preserving REM could blunt flare‑ups.
Practical Steps to Boost REM (and Potentially Reduce Pain)
- Consistent schedule: Go to bed and wake up at the same time daily. A regular rhythm stabilises the internal clock, encouraging full REM cycles.
- Limit blue light: Shut down phones, tablets, and TVs at least an hour before bedtime. Blue wavelengths suppress melatonin, delaying REM onset.
- Evening bright‑light exposure: 30 minutes of bright white or amber light (2,500-3,000 lux) after sunset can help phase‑advance REM, especially in shift‑workers.
- Mind‑body practices: Gentle yoga, progressive muscle relaxation, or mindfulness meditation before bed lower cortisol and promote deeper REM.
- Low‑dose melatonin: 0.3mg taken 30 minutes before sleep can shorten REM latency without causing grogginess.
- Avoid alcohol and heavy meals: Both disrupt REM architecture; alcohol especially cuts REM duration in the second half of the night.
- Create a cool, dark environment: A bedroom temperature of 16‑18°C (60‑65°F) and blackout curtains support the natural REM cycle.
These tweaks don’t replace medical pain treatment, but they give your body a better chance to harness REM’s natural analgesic effects.

When to Seek Professional Help
If you notice any of the following, it’s time to talk to a sleep or pain specialist:
- Pain spikes despite good sleep hygiene.
- Daily daytime fatigue that interferes with work or caring duties.
- Witnessed breathing pauses (possible sleep‑apnea) that also fragment REM.
- Medication side‑effects that may suppress REM (e.g., certain antidepressants).
An overnight polysomnography test can pinpoint REM deficits and guide targeted therapy. Treatment options range from CPAP for sleep‑apnea to cognitive‑behavioral therapy for insomnia (CBT‑I), both of which can restore REM and, indirectly, reduce pain.
Key Takeaway
While REM sleep won’t cure chronic pain outright, a healthy REM budget appears to lower pain sensitivity, calm inflammatory messengers, and rebalance hormones. By fine‑tuning bedtime habits, managing stress, and, when needed, seeking clinical assessment, you can turn a nightly rest into a potent ally against persistent aches.
Frequently Asked Questions
Can lack of REM cause chronic pain, or is it just a symptom?
Current research suggests a two‑way street. Poor REM can amplify pain pathways, but existing pain can also fragment sleep and cut REM. Breaking the cycle with better sleep hygiene often eases both.
How much REM do I need each night?
Adults typically spend about 20‑25% of total sleep time in REM, which translates to roughly 90‑110 minutes across a 7‑9 hour night.
Is melatonin safe for long‑term use to boost REM?
Low‑dose melatonin (0.3‑0.5mg) is generally considered safe for several months. Higher doses may cause daytime drowsiness and haven’t shown extra REM benefits.
Will exercise improve my REM and pain?
Regular moderate exercise (e.g., walking, swimming) performed earlier in the day can deepen overall sleep and modestly increase REM proportion, which may help reduce pain perception.
Can I track REM at home without a lab?
Wearable devices (e.g., advanced smartwatches) estimate REM using heart‑rate variability and motion data. They’re not as precise as polysomnography but give useful trends for personal adjustments.


Kevin Adams
October 17, 2025 AT 13:53Sleep is the silent teacher of our bodies the night whispers secrets about pain and healing! When REM slips away the nervous system rebels like a disgruntled poet refusing to rhyme and the aches bloom like shadows at dusk. The mind, drenched in dreams, tries to rewrite the story of suffering but without those rapid eye dances the script stays fractured. In this nightly theater the hormones play their part and the cytokines stage a revolt when the curtain falls too early. So remember, the darkness is not an enemy it is a canvas for the brain to paint relief if only we honor the REM hour!
Katie Henry
October 17, 2025 AT 16:06Dear readers, it is imperative to recognize that the quality of one's REM sleep can serve as a pivotal factor in the management of chronic pain. By adhering to a disciplined sleep schedule, reducing exposure to blue light, and incorporating evidence‑based practices such as low‑dose melatonin, you can actively influence neurochemical pathways that attenuate nociception. I encourage you to implement these strategies with confidence; consistent effort will undoubtedly yield measurable improvements in pain perception and overall well‑being.
Nickolas Mark Ewald
October 17, 2025 AT 17:30Sounds good. I try the same simple steps and noticed a small dip in my back aches after a week of steady bedtime.
Joanna Mensch
October 17, 2025 AT 20:16All this talk about melatonin being safe ignores the fact that big pharma pushes tiny doses while hiding the long‑term hormonal disruptions. The research they cite is funded by the same companies that sell synthetic sleep aids, so the “benefits” are often overstated. If you actually look at independent studies you’ll see mixed results and a pattern of data suppression. Trust your body’s natural rhythms instead of swallowing a pill that may be part of a larger agenda to keep us dependent on pharmaceuticals.
Sara Werb
October 17, 2025 AT 21:40Ugh, I hear you!!! The whole melatonin hype is just another scam cooked up in secret labs-don’t be fooled by those slick ads. They want us to think a tiny pill will fix everything while they harvest our data and our wallets. Stay woke, question the labels, and maybe try natural nighttime routines instead of buying into the corporate nightmare.
Chris Beck
October 17, 2025 AT 23:03Wake up and stop whining about REM!!
Russell Abelido
October 18, 2025 AT 01:50I've spent countless nights lying awake, feeling each ache as a reminder that my body is trying to tell me something, and I realized that REM sleep is more than just dreaming-it is a nightly negotiation between our mind and our pain receptors. When we allow ourselves the full arc of REM, the brain releases serotonin and dopamine, those gentle messengers that whisper “you are safe” to the spinal cord. In the absence of that restorative phase, the nervous system stays on high alert, amplifying even the tiniest pressure into a roaring storm. Think of REM as a skilled diplomat, calming the inflammatory cytokines that would otherwise wage war on our tissues. The studies cited in the article show that even a fifteen‑minute increase in REM can shift pain scores noticeably, which is nothing short of remarkable. Moreover, the hormonal ballet-melatonin cresting, cortisol descending-creates a landscape where inflammation cannot easily take root. By simply dimming the lights, avoiding alcohol, and perhaps taking a modest dose of melatonin, we grant the body the tools it needs to settle these internal disputes. I have personally tried a consistent bedtime routine, and over a month I observed a subtle but real easing of my fibromyalgia flare‑ups; the difference was like moving from a blaring alarm to a soft lullaby. It isn’t a miracle cure, but it is a powerful ally in the battle against chronic discomfort. 🌙😊
Remember, the journey to better sleep is a marathon, not a sprint; patience and persistence are key. Every night you invest in quality REM is a deposit into your pain‑management bank. So keep the bedroom cool, keep the mind calm, and let the night do its work. Your future self will thank you in quieter joints and clearer thoughts. 🙏 If you ever doubt the process, look back at the days when a restless night left you feeling like the whole world was in pain. The correlation between sleep architecture and pain perception is backed by neuroimaging that shows reduced activity in pain‑processing regions after REM‑rich sleep. Ultimately, embracing these habits empowers you to take control, rather than letting chronic pain dictate the terms of your life.
Steve Holmes
October 18, 2025 AT 03:13Yo, I dug into the light‑therapy tip and realized that a 30‑minute amber glow after sunset can actually shift your REM clock-crazy but true! It's simple, cheap, and you don't need fancy gadgets. Just set a lamp, chill for a bit, and let your body think it's still daytime in a good way. Give it a shot and watch how the morning aches start to ease.