Severe bleeding on medications isn't rare - it's a real, life-threatening risk
More than 1 in 3 people taking blood thinners will have some kind of bleeding problem within the first year. For some, it’s a small nosebleed. For others, it’s a hospital trip - or worse. The medications that keep your blood from clotting can also make it harder for your body to stop bleeding when something goes wrong. And when that bleeding becomes severe, every minute counts.
What counts as severe bleeding?
Severe bleeding isn’t just a lot of blood. It’s when your body can’t keep up. The medical definition is clear: a drop in hemoglobin of more than 5 g/dL, needing more than 4 units of blood transfusion, or bleeding that causes serious harm - like in the brain, spine, eyes, or gut. If you’re vomiting blood, coughing it up, or passing black, tarry stools, you’re not dealing with a minor issue. These aren’t symptoms you wait to see if they get better.
Even if you don’t see blood, warning signs matter. Dizziness, weakness, confusion, sudden severe headache, or swelling in a joint after a minor bump could mean internal bleeding. Many people ignore these signs because they don’t look like "bleeding." But in the case of anticoagulants, internal bleeding can be silent until it’s too late.
Which medications carry the highest risk?
All blood thinners increase bleeding risk, but not equally. Warfarin, the older drug, needs regular blood tests (INR) to keep the dose right. If your INR is too high, bleeding risk jumps fast. Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, dabigatran, and edoxaban don’t need routine testing - but they’re not safer. In fact, they’re responsible for more emergency visits now because more people are taking them.
Here’s what the data shows:
- Apixaban has the lowest annual major bleeding rate at 2.13%
- Rivaroxaban and dabigatran sit around 3.1-3.6%
- Warfarin is at 3.09%
But here’s the twist: 58% of bleeding events happen in patients on low-dose regimens. That’s not a mistake - it’s because those patients are often older, sicker, or have kidney problems. Dosing isn’t just about weight or condition. It’s about how your body handles the drug. And if your kidneys aren’t working well, the drug builds up. That’s why kidney function checks are non-negotiable before and during treatment.
Who’s most at risk?
You don’t have to be old to have a bleeding episode, but age is the biggest factor. People over 80 have more than 3 times the bleeding risk of those under 60. That’s not just because they’re frail - it’s because their kidneys slow down, their stomach lining gets more sensitive, and they’re more likely to be on multiple medications.
Other major risk factors:
- History of bleeding - if you’ve had a GI bleed before, your chance of another is 4.2 times higher
- Chronic kidney disease - doubles or triples your risk
- Taking aspirin or clopidogrel with your blood thinner - this combo doubles bleeding risk
- Uncontrolled high blood pressure - increases risk of brain bleeds
The HAS-BLED score is used by doctors to measure your personal risk. If your score is 3 or higher, your doctor should be discussing extra safety steps - not just handing you a prescription.

The first 90 days are the most dangerous
Half of all major bleeding events happen in the first three months. Why? Because your body is adjusting. Your doctor is still figuring out the right dose. And you’re still learning what symptoms mean.
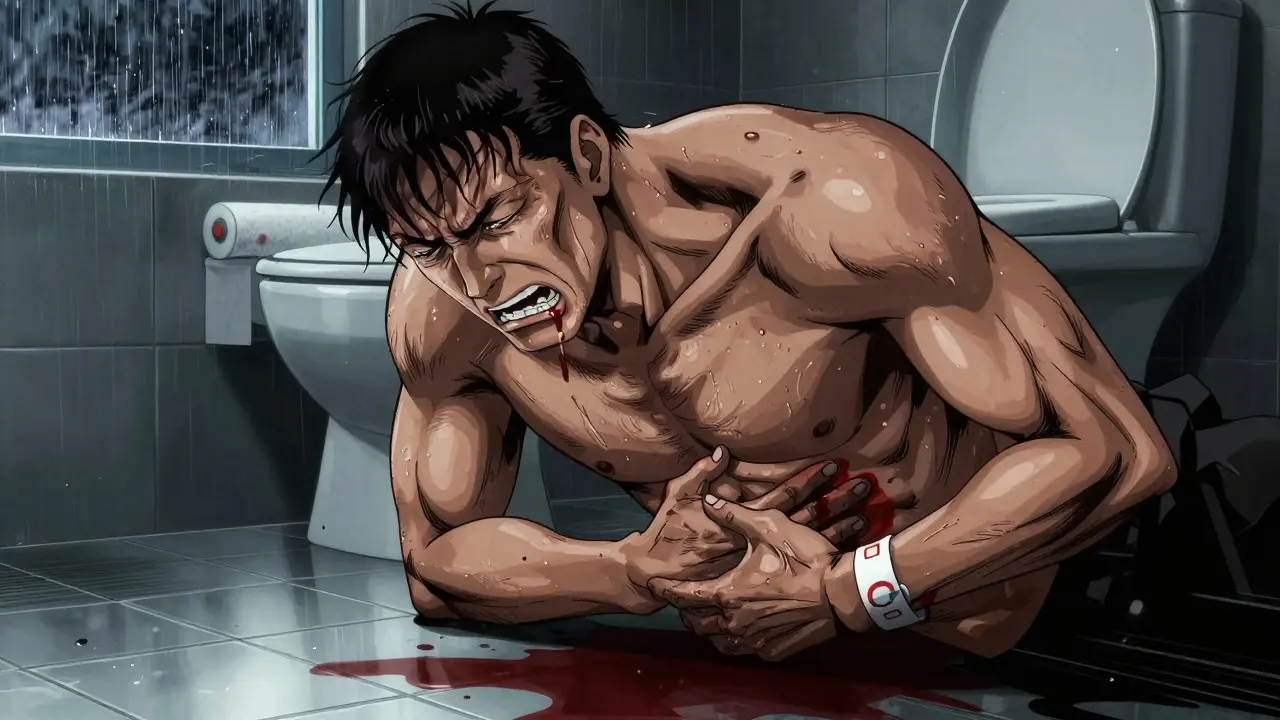
One patient on Reddit shared: "I took apixaban for six months. Started having black stools. Thought it was diet. Three days later, I passed out in the bathroom. They gave me two units of blood. I almost died."
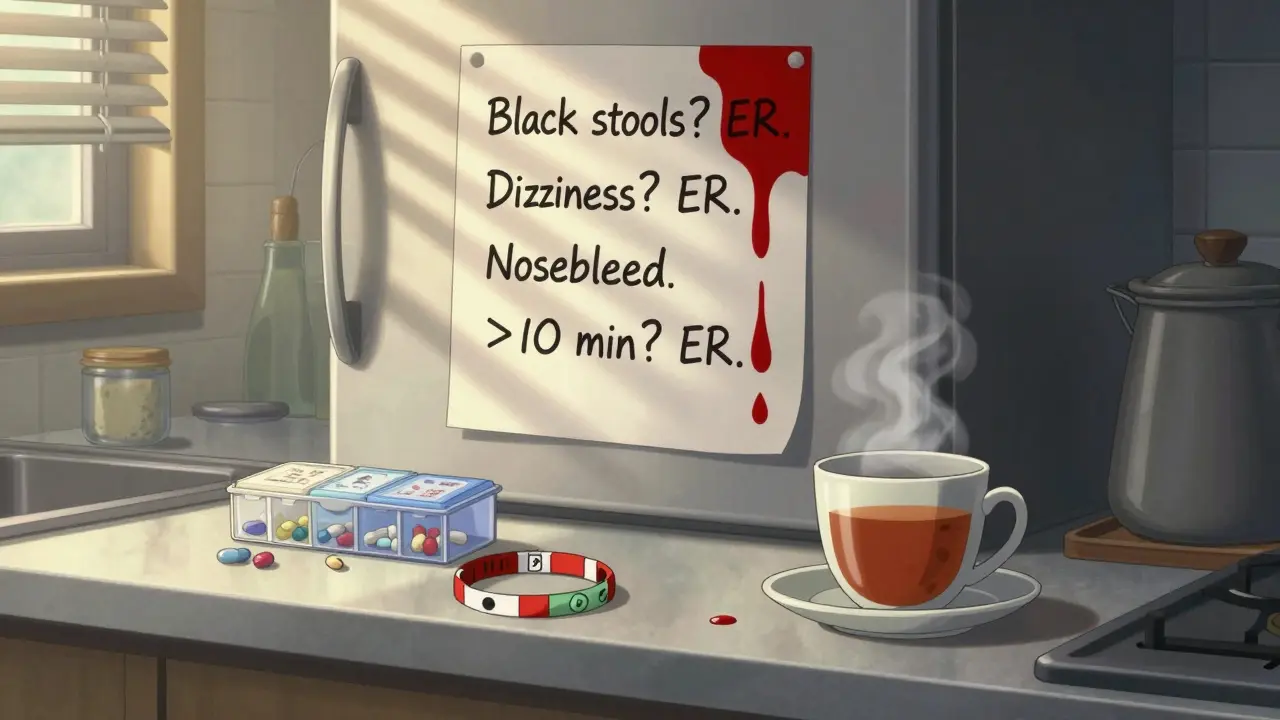
That’s not unusual. A Mayo Clinic survey found 28% of patients didn’t realize their symptoms were serious until it was too late. Nosebleeds that last more than 10 minutes? Go to the ER. Blood in urine? Don’t wait. Unexplained bruising that spreads? That’s not normal.
What to do if bleeding happens
There’s no time for hesitation. Here’s what to do immediately:
- Stop taking your blood thinner - don’t wait for a doctor’s call
- Call 999 or go to the nearest emergency department - don’t drive yourself if you’re dizzy or weak
- Bring your medication list - including exact names and doses
- Know your last dose - tell the ER team when you last took it
Don’t rely on symptoms to be dramatic. Internal bleeding doesn’t always bleed out. A small brain bleed might just feel like a bad headache. A slow gut bleed might only show up as fatigue. If you’re on a blood thinner and something feels "off," trust your gut.
Reversal agents exist - but they’re not always available
There are drugs that can undo the effects of blood thinners - but they’re expensive and not always in stock.
- For dabigatran: idarucizumab - costs around $3,500 per vial
- For rivaroxaban, apixaban, edoxaban: andexanet alfa - costs about $12,500 per treatment
In the UK, these aren’t routinely stocked in all hospitals. If you’re on a DOAC, ask your doctor: "What’s the plan if I bleed?" If they don’t have a clear answer, that’s a red flag.
For warfarin, vitamin K and fresh frozen plasma can reverse it - but it takes hours. With DOACs, reversal can happen in minutes - if the right drug is available.
What you can do to prevent bleeding
Prevention starts before you even take the pill.
- Get your kidney function tested before starting - creatinine clearance matters
- Review all your meds - NSAIDs like ibuprofen, aspirin, and even some herbal supplements (like ginkgo or garlic) can increase bleeding
- Ask for a bleeding risk score (HAS-BLED) - if it’s 3 or higher, ask for a safety plan
- Get a written emergency plan - symptoms to watch for, who to call, where to go
- Wear a medical alert bracelet - "On anticoagulant - risk of bleeding"
Patients who received a 15-minute safety talk at their first appointment were 34% less likely to delay going to the ER. That’s not a small number. It’s life-saving.
Why this is getting worse
The number of people on blood thinners has exploded. In the US, 10.2% of people over 65 are on them - up from 3.7% in 2010. More people = more bleeding events. In 2022, over 128,000 people in the US went to the ER because of anticoagulant bleeding - up 27% from 2018.
Doctors are prescribing more DOACs because they’re easier to manage. But easier doesn’t mean safer. And many patients aren’t being warned properly. The FDA now requires all DOAC labels to highlight the first-month bleeding risk. That’s progress. But it’s not enough.
What’s coming next
New drugs are in the pipeline. Milvexian and asundexian are two new anticoagulants in trials that show 20-25% less bleeding than current options - without losing protection against stroke. That’s huge.
Point-of-care tests are now approved to check DOAC levels in minutes, not days. That means doctors can adjust doses faster, especially for older patients or those with kidney issues.
But until these become standard, the responsibility falls on you. Know your risk. Know your symptoms. Know your emergency plan.
Final thought: Your life depends on knowing the difference between "normal" and "danger"
Anticoagulants save lives. But they can take them too - if you don’t know what to watch for. The goal isn’t to scare you off your medicine. It’s to make sure you’re not blindsided by a complication that could’ve been caught early.
If you’re on a blood thinner, print out the list of warning signs. Keep it on your fridge. Give a copy to a family member. Talk to your pharmacist. Ask your doctor: "What’s my bleeding risk? What’s the plan if something goes wrong?"
Because when it comes to severe bleeding, waiting to see if it gets better isn’t patience - it’s danger.
Can I stop my blood thinner if I start bleeding?
Yes - stop taking it immediately and go to the emergency room. Do not wait to call your doctor first. Delaying care increases the risk of serious harm or death. Once you’re in the hospital, the medical team will decide if and when to restart the medication.
Is it safe to take ibuprofen or aspirin with a blood thinner?
No - not without your doctor’s approval. Both ibuprofen and aspirin increase bleeding risk, especially in the stomach. Even low-dose aspirin can double your chance of a GI bleed when taken with a DOAC or warfarin. Use paracetamol (acetaminophen) for pain instead, and always check with your pharmacist before taking any new medication.
How do I know if my nosebleed is serious?
If it lasts longer than 10 minutes despite pinching your nose and leaning forward, or if you’re swallowing a lot of blood, feeling dizzy, or getting weak - go to the ER. A nosebleed that won’t stop can be a sign your blood is too thin. Don’t assume it’s just a dry nose.
Do I need blood tests if I’m on a DOAC like apixaban?
Routine blood tests aren’t required for DOACs - but they’re still important. Your doctor should check your kidney function every 3-6 months. If you’re over 75, have kidney disease, or have had bleeding before, some clinics now use point-of-care tests to measure drug levels. Ask if this is right for you.
Can I still exercise or play sports on blood thinners?
Yes - but avoid high-risk activities like contact sports, skiing, or rock climbing. Low-impact exercise like walking, swimming, and cycling is safe and encouraged. Always wear protective gear if there’s any chance of falling or bumping into something. A minor fall can turn into a major bleed.
What should I do if I forget to take my blood thinner?
If you miss a dose, take it as soon as you remember - but only if it’s within 6 hours of your usual time. If it’s been longer, skip the missed dose and take your next one at the regular time. Never double up. Missing doses increases clot risk, but doubling up increases bleeding risk. Talk to your doctor or pharmacist about your specific medication’s guidelines.
Is there a way to test my blood thinner level at home?
For warfarin, yes - home INR monitors are available and covered by the NHS in some cases. For DOACs, home testing isn’t yet available. But point-of-care DOAC level tests are now approved and being rolled out in hospitals. Ask your clinic if they offer this for high-risk patients.
Next steps: What to do today
- If you’re on a blood thinner, review your bleeding risk with your doctor - ask for your HAS-BLED score
- Make sure you have a written emergency plan - symptoms, who to call, where to go
- Check your kidney function - get a recent blood test if it’s been over 6 months
- Remove NSAIDs from your medicine cabinet - switch to paracetamol for pain
- Wear a medical alert bracelet - it could save your life

Manan Pandya
December 29, 2025 AT 18:55Emma Duquemin
December 31, 2025 AT 15:39Aliza Efraimov
December 31, 2025 AT 17:23Nisha Marwaha
January 2, 2026 AT 12:49Russell Thomas
January 3, 2026 AT 02:43Joe Kwon
January 4, 2026 AT 16:37Teresa Rodriguez leon
January 4, 2026 AT 17:46Paige Shipe
January 6, 2026 AT 06:01Tamar Dunlop
January 7, 2026 AT 16:45Duncan Careless
January 8, 2026 AT 08:50