SGLT2 inhibitors are no longer just another diabetes pill. For people with type 2 diabetes-especially those with heart or kidney problems-they’ve become one of the most important treatment options available today. Unlike older drugs that just push sugar out of the blood, these medications work in the kidneys to flush excess glucose into urine. But their real power isn’t just in lowering A1c. They cut heart failure hospitalizations, slow kidney damage, and even help with weight loss-all without causing dangerous low blood sugar. Still, they’re not risk-free. Genital infections, dehydration, and rare but serious conditions like diabetic ketoacidosis can happen. If you’re considering one, you need to know both sides.
How SGLT2 Inhibitors Actually Work
These drugs block a protein in your kidneys called SGLT2. Normally, this protein grabs glucose from your urine and sends it back into your bloodstream. When you take an SGLT2 inhibitor, that process stops. Instead of reabsorbing sugar, your kidneys dump it out-about 40 to 100 grams a day. That’s like losing the sugar from two cans of soda every day through your pee.
This mechanism means blood sugar drops without forcing your pancreas to pump out more insulin. That’s why you rarely get low blood sugar unless you’re also taking insulin or sulfonylureas. It also explains the weight loss: you’re literally peeing out calories. Most people lose 2 to 3 kilograms in the first few months. Blood pressure tends to drop too, by 3 to 5 mmHg, because less fluid stays in your body.
The four main SGLT2 inhibitors on the market are canagliflozin (Invokana), dapagliflozin (Farxiga), empagliflozin (Jardiance), and ertugliflozin (Steglatro). Each works the same way, but their dosing and how they’re cleared from the body differ. For example, empagliflozin is mostly removed by the liver, while dapagliflozin relies more on the kidneys. That matters if your kidney function is already low.
Proven Benefits Beyond Blood Sugar
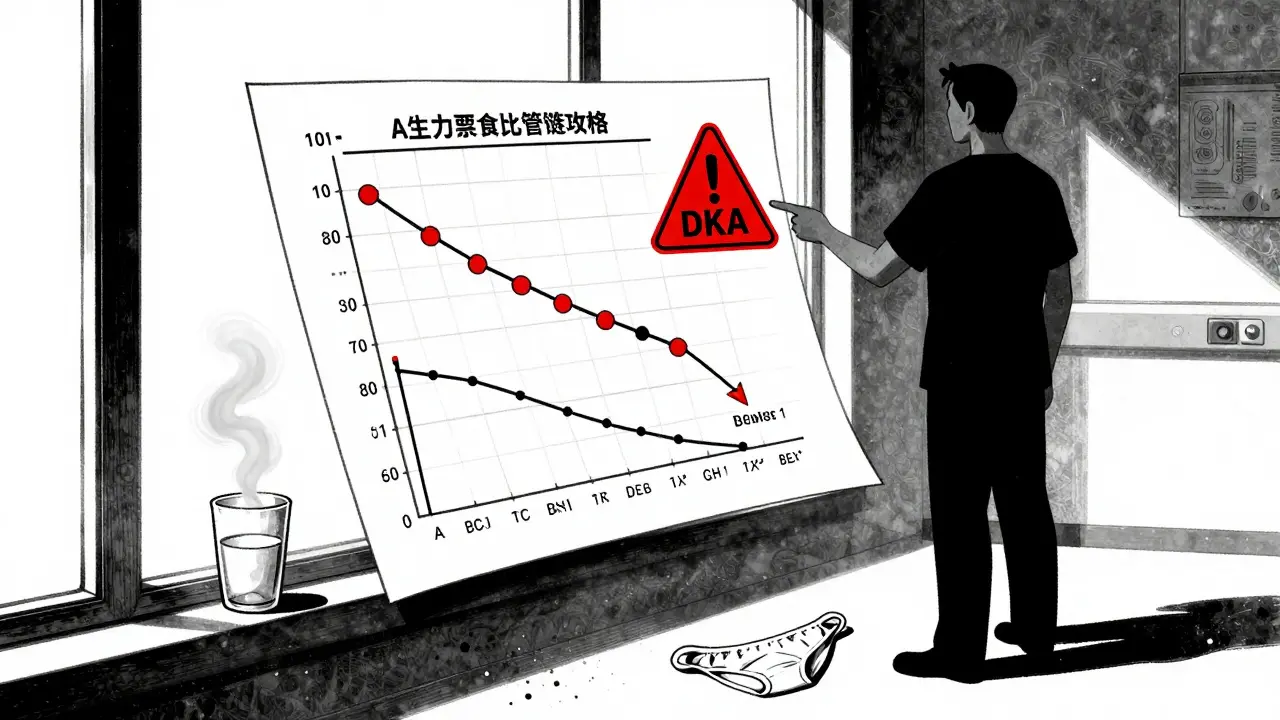
What changed everything was the big clinical trials. Before 2015, these drugs were seen as backup options. Then came EMPA-REG OUTCOME, CANVAS, and DECLARE-TIMI 58-massive studies with over 60,000 patients. The results shocked doctors.
Empagliflozin cut cardiovascular death, heart attack, and stroke by 14%. Canagliflozin did the same. Dapagliflozin slashed hospital stays for heart failure by 17%. These weren’t small wins. They were life-saving.
But the biggest surprise? Their effect on kidneys. The CREDENCE trial showed canagliflozin reduced the risk of kidney failure, needing dialysis, or dying from kidney disease by 30%. The DAPA-CKD and EMPA-KIDNEY trials later proved dapagliflozin and empagliflozin work even in people without diabetes who have chronic kidney disease. That’s why the FDA approved dapagliflozin in 2023 for kidney protection regardless of diabetes status.
Heart failure benefits extend beyond type 2 diabetes. In patients with heart failure and reduced ejection fraction (HFrEF), SGLT2 inhibitors reduced hospitalizations by 30% to 35%. Even in those with preserved ejection fraction, dapagliflozin lowered risk by 18%. These drugs now have a Class 1 recommendation from the American College of Cardiology for heart failure patients-whether they have diabetes or not.
Who Should Be Taking Them
Current guidelines from the American Diabetes Association (2023) say SGLT2 inhibitors should be first-line for people with type 2 diabetes who have:
- Established heart disease (like a past heart attack or angina)
- Heart failure (even if it’s mild)
- Chronic kidney disease (eGFR ≥30)
If you have any of these, you’re not just treating diabetes-you’re protecting your heart and kidneys. That’s a game-changer.
Even if you don’t have those conditions yet, but you’re at high risk-say, you’re overweight, have high blood pressure, or a family history of heart disease-these drugs might still be worth considering. The number needed to treat to prevent one major heart event over five years is 52 for low-risk patients, which is less impressive than the 17 needed for those with prior heart attacks. But for some, the long-term protection justifies the cost.
They’re not for everyone. They’re not approved for type 1 diabetes. They’re not recommended if your eGFR is below 30. And they’re not first-choice for someone with no heart, kidney, or weight issues who just needs to lower A1c by 0.5%.
The Risks You Can’t Ignore
These drugs are powerful, but they come with real side effects. The most common? Genital yeast infections. Up to 11% of women and 5% of men report them. They’re not dangerous, but they’re annoying-itching, burning, discharge. Many patients stop taking the drug because of this. Good hygiene and wearing cotton underwear help. If infections keep coming back, talk to your doctor about switching.
Urinary tract infections are also more common, though less frequent than yeast infections. If you get frequent UTIs, especially with fever or back pain, don’t ignore it. SGLT2 inhibitors can make them worse.
The scariest risk? Diabetic ketoacidosis (DKA). This is rare-only 0.1% to 0.3% of users-but it can be deadly. What’s different here is euglycemic DKA. Your blood sugar might only be 180-250 mg/dL-not the 400+ you’d expect. That’s dangerous because you won’t realize you’re in trouble until you’re vomiting, breathing fast, or confused. This happens more during illness, fasting, surgery, or heavy drinking. If you’re sick, hold your SGLT2 inhibitor and call your doctor. Never restart it without checking your ketones first.
Another rare but serious risk is Fournier’s gangrene-a life-threatening infection of the genitals and perineum. The FDA added a black box warning for this in 2018. It’s extremely rare (0.002%), but it’s happened. If you notice swelling, pain, redness, or fever in your genital area, go to the ER immediately.
Some people get dehydrated, especially older adults or those on diuretics. That can lead to dizziness, low blood pressure, or even acute kidney injury. The FDA has a black box warning for this too. Drink water. Avoid alcohol. Watch for signs like dry mouth, dark urine, or feeling lightheaded when standing up.
Canagliflozin has a slightly higher risk of lower limb amputation-mostly toes and feet. The CANVAS trial showed a 1.97 times higher risk. It’s not common, but if you have foot ulcers, neuropathy, or poor circulation, your doctor might avoid this one.
Cost and Accessibility
These drugs are expensive. A 30-day supply costs around $600 out-of-pocket. That’s why many patients stop after six months. But most insurance plans cover them, and manufacturer programs can bring your monthly cost down to $10-$25. If you’re struggling to afford it, ask your pharmacist about patient assistance programs. Don’t skip doses because of cost-talk to someone who can help.
There are no generics yet. Patents run until 2027-2029. Until then, you’re paying brand prices. Some patients switch to GLP-1 agonists like semaglutide, which offer similar heart and weight benefits-but those are even more expensive and require injections.
What to Expect When Starting
If your doctor prescribes one, here’s what happens:
- You’ll get a baseline eGFR test. If it’s below 45, your dose might be lowered.
- You’ll be told to drink more water, especially in hot weather or when exercising.
- You’ll get instructions on how to handle illness: hold the drug if you’re vomiting, have a fever, or can’t eat.
- You’ll be warned about genital hygiene and signs of infection.
- You’ll check your blood sugar more often at first, especially if you’re also on insulin.
Most people feel fine. Some notice more frequent urination at first-it’s normal. Weight loss starts in 2-4 weeks. A1c drops by 0.6% to 0.8% in three months. If you’re losing weight and feeling better, that’s a good sign. If you’re dizzy, itchy, or sick, call your doctor.

How They Compare to Other Diabetes Drugs
Compared to metformin, SGLT2 inhibitors don’t cause stomach upset but are more expensive. They’re better for heart and kidney protection.
Compared to DPP-4 inhibitors (like sitagliptin), SGLT2 inhibitors offer more weight loss and better heart failure outcomes. DPP-4s are neutral on weight and have no proven heart benefit.
Compared to GLP-1 agonists (like semaglutide), SGLT2 inhibitors are pills, not injections. They’re slightly less effective for weight loss and A1c reduction, but better for heart failure. GLP-1s win on preventing heart attacks and strokes.
There’s no perfect drug. But for people with heart or kidney disease, SGLT2 inhibitors are among the best tools we have.
Real Stories, Real Outcomes
A 58-year-old man in Ohio switched from metformin to Jardiance after a heart attack. His ejection fraction went from 28% to 42% in 18 months. He hasn’t been hospitalized since.
A 62-year-old woman in Texas stopped Farxiga after six months because of recurring yeast infections. She says her blood sugar was great, but the discomfort wasn’t worth it.
A Reddit user lost 15 pounds in three months on Farxiga. His A1c dropped from 8.2 to 6.8. He didn’t change his diet. He just took the pill.
These aren’t outliers. They’re what happens when the science meets real life.
Final Thoughts
SGLT2 inhibitors aren’t magic. But they’re one of the few diabetes drugs that actually change the course of the disease-not just manage symptoms. If you have type 2 diabetes and heart or kidney problems, they should be on your radar. If you’re healthy and just need to lower A1c, there might be cheaper, simpler options.
Ask your doctor: Do I have heart or kidney disease? Am I at high risk? Will this drug protect me beyond my blood sugar? Don’t just accept a prescription. Understand why it’s being offered.
And if you’re worried about side effects-talk about them. Genital infections are common, but treatable. Dehydration is preventable. Ketoacidosis is rare, but you need to know the signs. Knowledge turns fear into control.