When you pick up a prescription, you might not realize the pharmacy benefit manager, a middleman between drug makers, insurers, and pharmacies that negotiates prices and manages drug lists. Also known as PBM, it decides which drugs are covered, how much you pay at the counter, and which pharmacies you can use. Most people don’t know PBMs exist—until they get a bill they didn’t expect, or their doctor’s prescribed drug isn’t on the list.
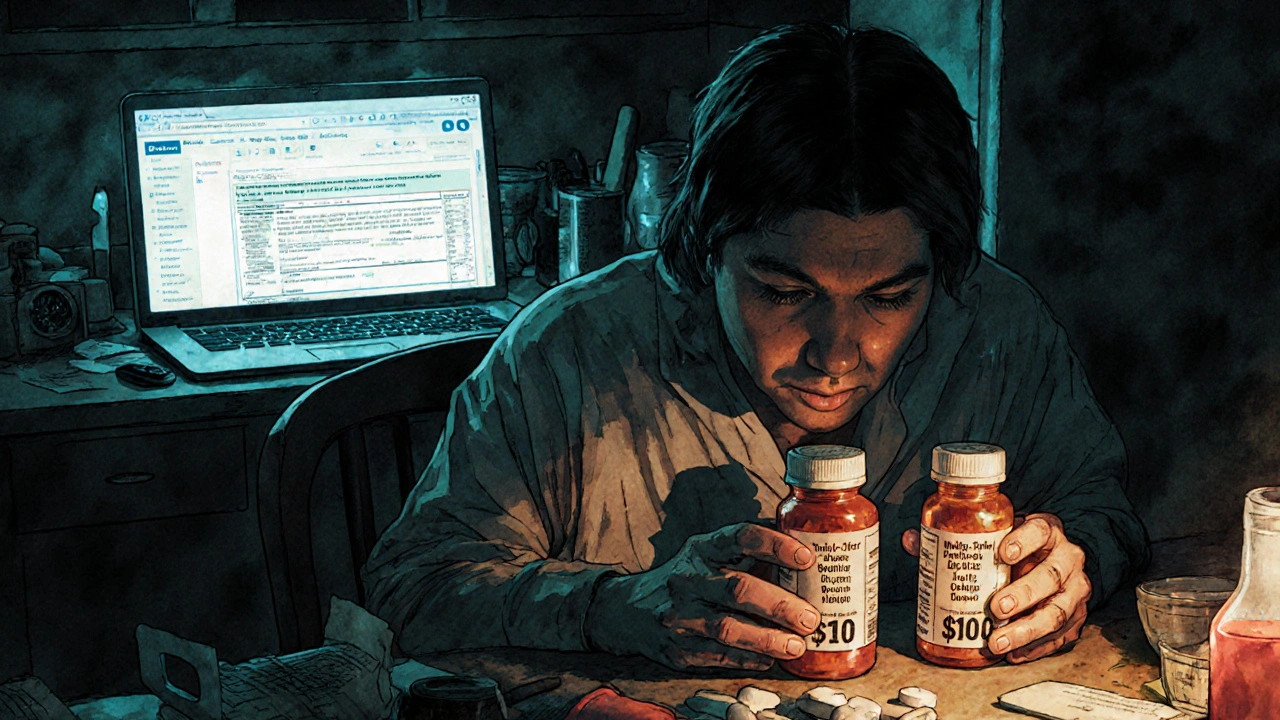
PBMs don’t make drugs. They don’t treat patients. But they control access to them. They strike deals with drug companies: if a manufacturer gives a big discount, the PBM puts that drug on its preferred list. If not, it gets pushed to the back, or blocked entirely. That’s why two people with the same insurance might pay wildly different prices for the same pill. One’s PBM has a deal with the maker; the other’s doesn’t. And when a drug gets moved to a higher tier, your out-of-pocket cost can jump from $10 to $200 overnight—no warning, no explanation.
These companies also run mail-order pharmacies, own retail chains, and collect rebates that aren’t always passed to you. A PBM might get $50 back from a drugmaker for every prescription filled, but you still pay the full list price at the counter. That’s the gap between the sticker price and what your plan actually pays. And because PBMs are often owned by big insurers like CVS Health or UnitedHealthcare, the same company that sets your premiums also controls your drug access. It’s not a conflict of interest—it’s the business model.
What does this mean for you? If you’re on a long-term medication, your PBM can change your drug’s status at any time. Your doctor might prescribe a drug you’ve used for years, but if the PBM drops it from the formulary, you’ll get a denial notice. You might need prior authorization, step therapy (try cheaper drugs first), or switch to a generic. Sometimes, the generic isn’t even made by the same company—it’s a different formula, with different side effects. And if you live in a rural area, your local pharmacy might not be in the PBM’s network, forcing you to ship pills by mail or drive miles out of town.
That’s why the posts below matter. They don’t just talk about drugs—they show you how the system works behind the scenes. You’ll find guides on drug pricing, how list prices are set, what rebates really mean, and why your copay doesn’t reflect the real cost. You’ll see how insurance pharmacy networks, the list of pharmacies your PBM allows you to use can leave you stranded. You’ll learn how to challenge a PBM denial, how to spot when you’re being overcharged, and how to find cheaper alternatives that your plan actually covers.
This isn’t about blaming PBMs. It’s about understanding them. Because if you don’t know how they operate, you’re leaving money on the table—and maybe even your health at risk. The posts here give you the tools to navigate the system, not just accept it. Whether you’re paying for statins, insulin, or an ED pill, what you pay isn’t random. It’s decided by someone you’ve never met. Now you know who they are, and what they control.
Learn how insurance covers generic drugs from online pharmacies in 2025 - including mail-order vs. independent sites, copay tricks, Amazon RxPass, and what to do when your insurer forces a switch.
Read More >>