When you see a verify medication warning, a clear signal from regulators or manufacturers that a drug carries serious, potentially life-threatening risks. Also known as black box warning, it doesn’t mean stop taking the medicine—it means understand the risk, know the signs, and talk to your doctor before making any changes. These warnings aren’t scare tactics. They’re based on real data from thousands of patients, and they’re there because someone, somewhere, almost didn’t make it.
These alerts don’t appear randomly. They’re tied to specific drugs that have shown dangerous side effects in clinical use. For example, black box warning, the strongest safety alert the FDA can issue. Also known as FDA boxed warning, it’s used when a drug can cause severe reactions like heart rhythm problems, liver failure, or dangerous bleeding. You’ll find these on medications like blood thinners, antipsychotics, or even some antibiotics. They’re printed in bold black borders on the label because the risk isn’t theoretical—it’s been documented in hospitals and ERs.
But a warning isn’t the same as a ban. Many people live safely with these drugs because they’re monitored. A drug safety, the practice of tracking and managing risks linked to medications. Also known as pharmaceutical safety, it includes everything from lot number tracking to patient alerts. system helps catch fake pills before they reach you. Lot numbers and serial codes let pharmacies and regulators trace every pill back to its factory. If a batch is recalled, you’re notified. If a drug is found to be contaminated or ineffective, you’re protected.
And it’s not just about the pill itself. Your body’s condition matters too. A statin might be safe for most, but if you’re pregnant or have liver disease, the risk changes. A blood thinner might save your life after a stroke—but if you fall and hit your head, that same drug could turn a minor injury into a crisis. That’s why medication alerts, personalized reminders tied to your health history and prescriptions. Also known as drug interaction alerts, they’re built into pharmacy systems and medical records. aren’t just for doctors. You need to know your own triggers: Are you on more than three pills? Are you over 65? Do you take herbal supplements? Each of those adds layers to the warning.
Some warnings are obvious—like the one on warfarin about bleeding. Others are hidden in plain sight. A sedating antihistamine might help you sleep, but for older adults, it can trigger a fall that breaks a hip. A QT-prolonging combo might not show up on a basic blood test, but it can cause sudden cardiac arrest. That’s why verifying isn’t a one-time check. It’s an ongoing conversation—with your pharmacist, your doctor, even your family.
Below, you’ll find real stories and clear guides on how to read these warnings, what to do when you see them, and how to protect yourself without stopping the treatment you need. Whether it’s about expired pills, counterfeit drugs, or hidden interactions, the goal is the same: help you stay safe without living in fear.
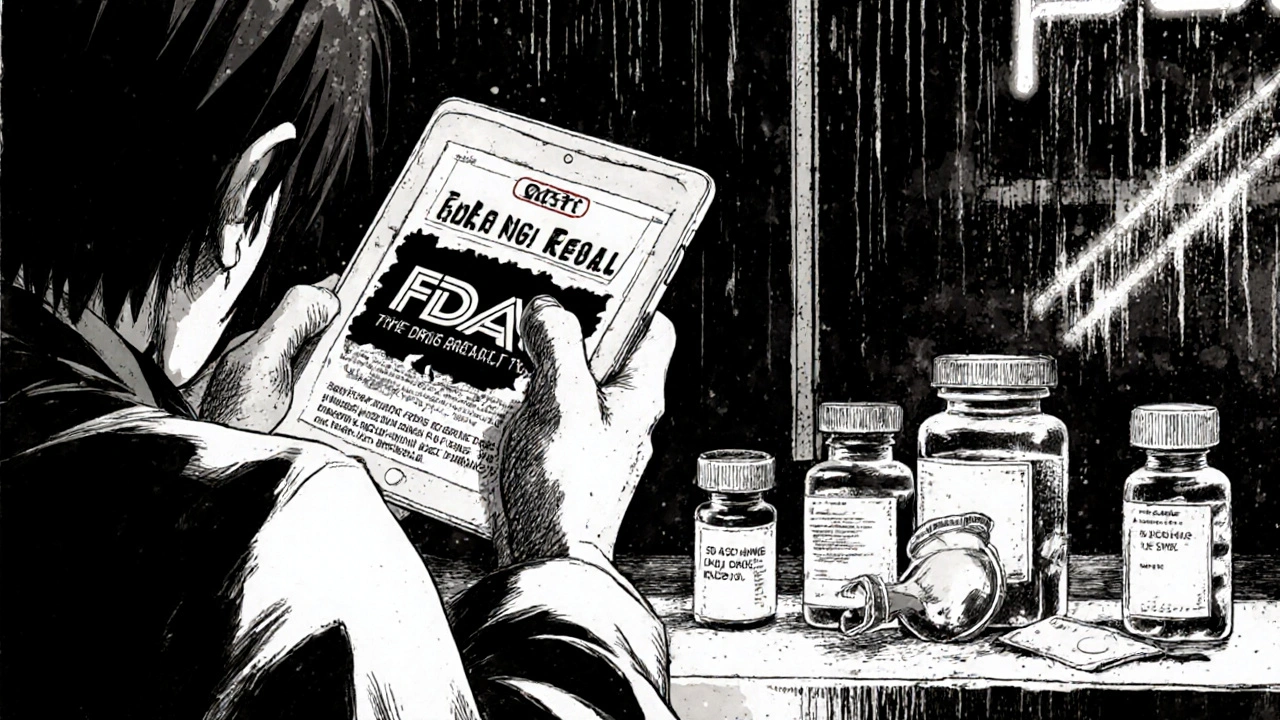
Learn how to verify real drug recalls from fake ones online. Avoid dangerous mistakes by checking official FDA sources, lot numbers, and recall codes before stopping your medication.
Read More >>