When you hear the word thyroid, you might think of weight changes, fatigue, or mood swings. But behind those symptoms often lies something invisible: nodules. These small lumps in the thyroid gland are surprisingly common - found in up to 68% of people who get an ultrasound, even if they feel perfectly fine. The real question isn’t whether you have a nodule. It’s whether it’s dangerous. And that’s where thyroid ultrasound comes in.
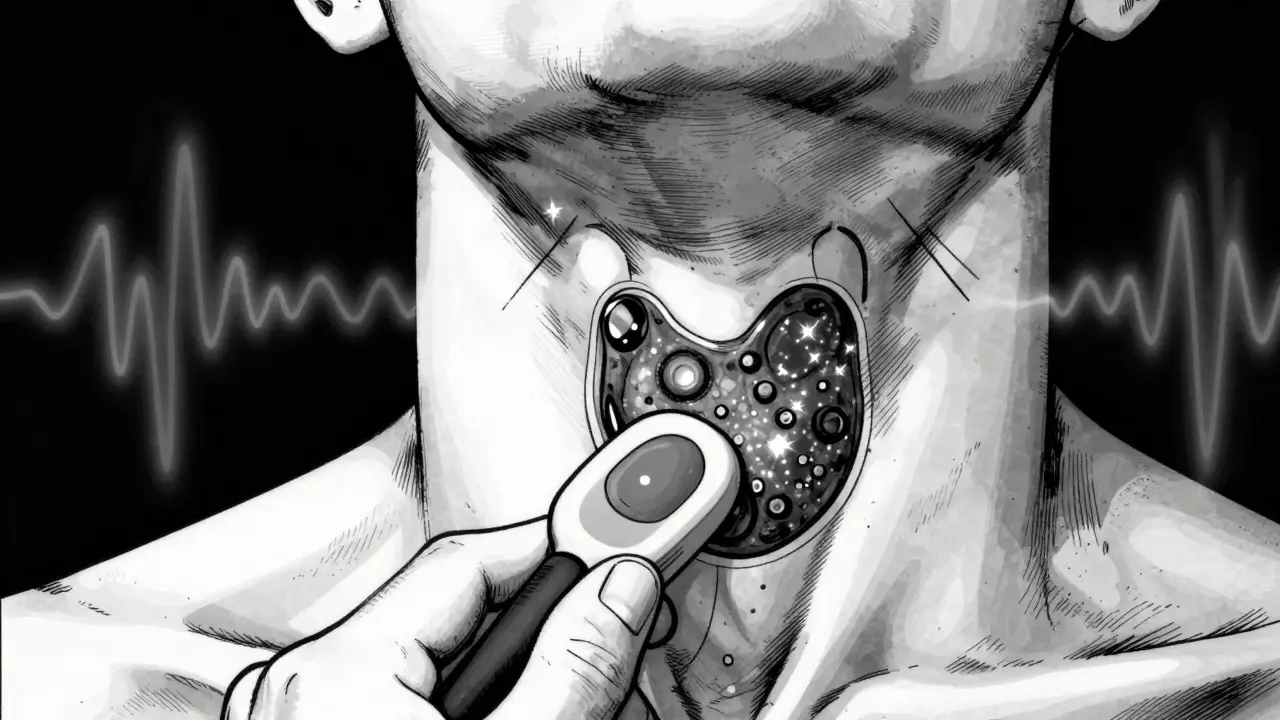
What Thyroid Ultrasound Actually Shows
Thyroid ultrasound doesn’t use radiation. It doesn’t involve needles or contrast dye. It uses sound waves - the same kind used during pregnancy scans - to create a real-time video of your thyroid. A technician moves a small handheld device (a transducer) over your neck, and the machine turns the returning echoes into a detailed image. This lets doctors see the size, shape, and internal structure of every nodule.
Not all nodules are the same. Some are filled with fluid (cysts), others are spongy and full of tiny holes (spongiform), and some are solid masses. The key is spotting the ones that look suspicious. For example, a nodule that’s solid, darker than surrounding tissue (hypoechoic), and shaped taller than wide raises red flags. So do tiny white dots inside - called microcalcifications - which are often signs of early cancer.
Modern ultrasound machines also show blood flow. A nodule with blood vessels running through its center (central vascularity) is more likely to be cancerous than one with blood around its edges. These aren’t guesses. They’re patterns backed by decades of research and confirmed in hundreds of thousands of cases.
The TI-RADS System: Your Nodule’s Risk Score
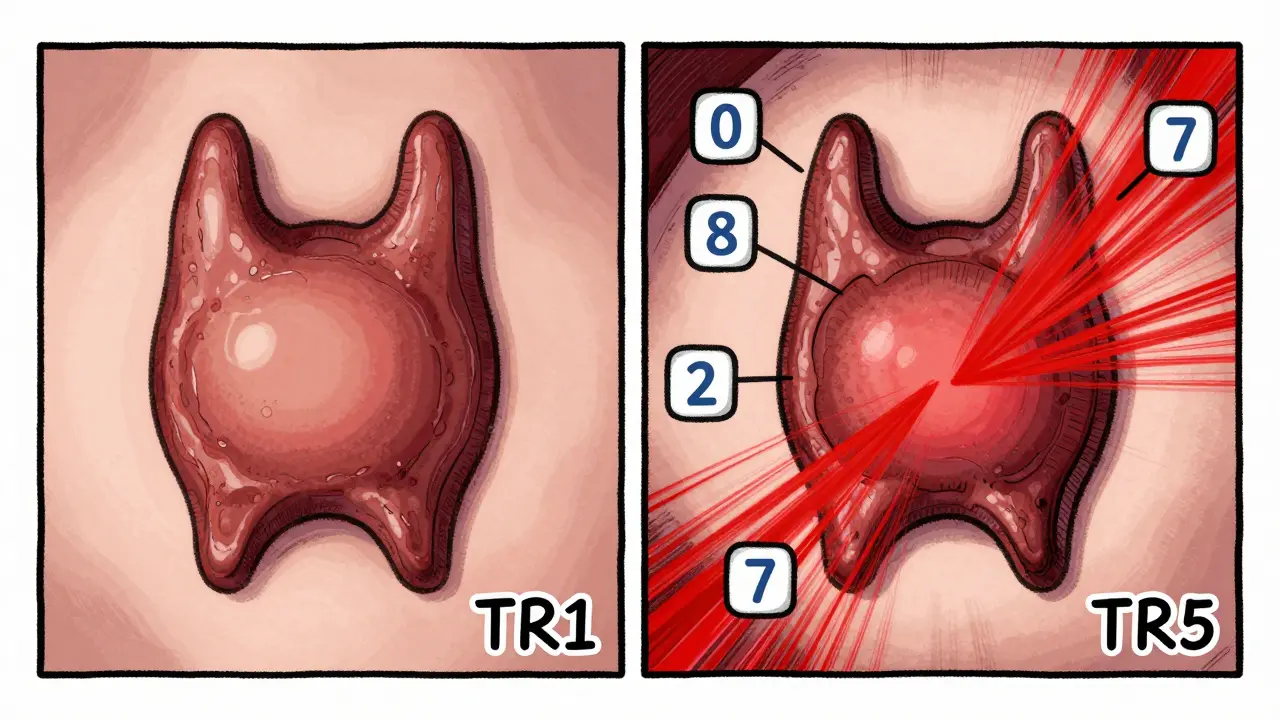
In 2017, the American College of Radiology created TI-RADS - short for Thyroid Imaging Reporting and Data System. Think of it like a traffic light for thyroid nodules. Each nodule gets scored based on five features:
- Composition: Is it mostly fluid, spongy, mixed, or solid?
- Echogenicity: How bright or dark does it look compared to normal thyroid tissue?
- Shape: Is it wider than tall (good) or taller than wide (bad)?
- Margin: Are the edges smooth or jagged, with signs of spreading outside the gland?
- Echogenic foci: Are there microcalcifications inside?
Each feature gets 0 to 3 points. Add them up, and you get a TI-RADS category:
- TR1 (0 points): 0.3% cancer risk - essentially harmless.
- TR2 (2 points): 1.5% risk - still very low.
- TR3 (3 points): 4.8% risk - mildly suspicious.
- TR4 (4-6 points): 9.1% risk - moderate concern.
- TR5 (7+ points): 35% risk - high chance of cancer.
This system replaced older, less consistent methods. Studies show TI-RADS is far better at predicting which nodules need biopsy. A nodule with a TR5 score isn’t cancer yet - but it’s risky enough that doctors almost always recommend a biopsy.
Why Ultrasound Beats Other Tests
You might wonder: Why not just do a CT scan or MRI? Those can show nodules too. But they miss the details that matter.
CT and MRI are great for big structures - like tumors pressing on your windpipe. But they can’t see microcalcifications. They can’t tell if a nodule is taller than wide. They don’t show blood flow patterns. And they expose you to radiation.
Nuclear scans (like radioactive iodine uptake tests) tell you if a nodule is “hot” (overactive) or “cold” (underactive). Hot nodules almost never turn cancerous. Cold ones have about a 15% risk. But that’s still a guess. Ultrasound gives you the real picture - not just whether the nodule is active, but what it looks like inside.
Ultrasound is also the only way to guide a fine-needle biopsy. Without it, doctors might miss the nodule entirely or sample the wrong part. With ultrasound guidance, the chance of getting a useless sample drops from 25% to under 5%.
When Do You Need a Biopsy?
Not every nodule needs a biopsy. Size matters - but not as much as appearance.
- Nodules under 5 mm: No follow-up needed, even if they look suspicious. They’re too small to be dangerous.
- Nodules 1 cm or larger with TR4 or TR5 features: Biopsy is recommended.
- Nodules 2.5 cm or larger with TR3 features: Biopsy is still advised. Studies show cancer survival isn’t affected until tumors reach this size.
Even if a biopsy comes back as “indeterminate” - meaning it’s unclear if it’s cancer - you’re not done. About 15-30% of biopsies land in this gray zone. That’s where molecular testing helps. Tests like Afirma or ThyroSeq can now tell you with high accuracy whether the nodule is likely benign. If they say “benign,” you can skip surgery. But you still need regular ultrasounds to watch for changes.
The Rise of AI in Ultrasound
AI isn’t replacing radiologists - it’s helping them. A 2023 study in Nature Scientific Reports tested a deep learning model that analyzed thousands of thyroid ultrasounds. It looked at nodule shape, texture, and even subtle patterns invisible to the human eye. The AI reached 94.2% accuracy in spotting cancer - higher than most human experts.
Why does this matter? Because reading ultrasounds is hard. Studies show even experienced radiologists disagree on margin shape or echogenicity about 30-40% of the time. AI helps standardize that. It doesn’t make the call - but it flags the high-risk features so the doctor doesn’t miss them.
By 2024, the American College of Radiology plans to update TI-RADS to include AI-assisted features. The goal? To combine imaging data with molecular markers and create personalized risk scores. Imagine a system that says: “Your nodule has a 7% cancer risk based on its shape, blood flow, and genetic profile.” That’s the future - and it’s already starting.

What’s Not Being Done - and Why It Matters
Here’s the scary part: nearly one in three community ultrasounds don’t check the lymph nodes in the neck. That’s a critical mistake. Thyroid cancer often spreads first to nearby lymph nodes. If those aren’t examined, you might miss early signs of spread.
Also, many clinics still use old ultrasound machines with low-frequency transducers (below 10 MHz). These can’t capture fine details. The American Institute of Ultrasound in Medicine recommends at least 10 MHz for thyroid imaging. If your scan was done on an old machine, it might not be reliable.
And then there’s the issue of over-testing. Not every thyroid nodule needs to be scanned. If you have no symptoms, no family history, and normal thyroid blood tests, routine screening isn’t recommended. But if you’ve had radiation exposure, a family history of thyroid cancer, or you’re over 50 - ultrasound is a smart first step.
What Happens After the Scan?
If your nodule is low-risk (TR1 or TR2), you’ll likely just get a repeat ultrasound in 1-2 years. No surgery. No medication. Just watchfulness.
If it’s high-risk (TR5), you’ll probably be referred for a biopsy. If cancer is confirmed, many patients - especially those with small, slow-growing tumors - don’t need surgery right away. Active surveillance is now a standard option. Studies show that for tumors under 1 cm, 10-year survival is over 99% with monitoring alone. Surgery isn’t always the answer.
Even after treatment, ultrasound remains key. It’s used to check for recurrence, track lymph nodes, and monitor the other side of the thyroid. It’s not a one-time test. It’s part of long-term care.
Thyroid ultrasound isn’t magic. It doesn’t diagnose cancer on its own. But it gives you the clearest, safest, most detailed picture of what’s happening inside your neck. And in a world where early detection saves lives, that’s worth more than any other test.
Can thyroid ultrasound detect cancer for sure?
No. Ultrasound can only identify features that suggest cancer - like microcalcifications, irregular shape, or central blood flow. Only a biopsy can confirm whether a nodule is cancerous. Ultrasound helps decide which nodules need a biopsy, but it doesn’t replace it.
Is thyroid ultrasound painful or risky?
It’s completely painless and safe. No radiation, no needles, no contrast dye. You lie on your back, a gel is applied to your neck, and the technician moves a small probe over the area. It takes 15-30 minutes. There are no known risks.
How accurate is TI-RADS in predicting cancer?
TI-RADS is highly accurate. Studies show it correctly identifies cancer risk in over 90% of cases. A TR5 nodule has a 35% chance of being cancerous - meaning it’s the most reliable predictor available. TR1 and TR2 nodules have less than 2% risk, so they rarely require biopsy.
Do all thyroid nodules need treatment?
No. Over 90% of thyroid nodules are benign and don’t need treatment. Even some small cancers (under 1 cm) can be safely monitored without surgery. Treatment - whether medication, biopsy, or surgery - is only recommended if the nodule is large, growing, suspicious, or causing symptoms.
Can I get thyroid ultrasound without a doctor’s referral?
In most cases, no. Ultrasound is a diagnostic tool, not a screening test for healthy people. You typically need a referral from a doctor based on symptoms, blood tests, or physical findings. Routine screening for nodules in asymptomatic people isn’t recommended.