If you’ve tried CPAP for sleep apnea and gave up because of the mask, the noise, or the discomfort, you’re not alone. About 3 in 10 people abandon CPAP within the first year. But what if there was another way-one that doesn’t involve a hose, a mask, or nightly frustration? Upper airway stimulation (UAS), specifically the Inspire therapy, is a surgically implanted device that quietly keeps your airway open while you sleep. It’s not for everyone, but for those who’ve tried everything else, it’s changed their lives.
How It Works: A Pacemaker for Your Airway
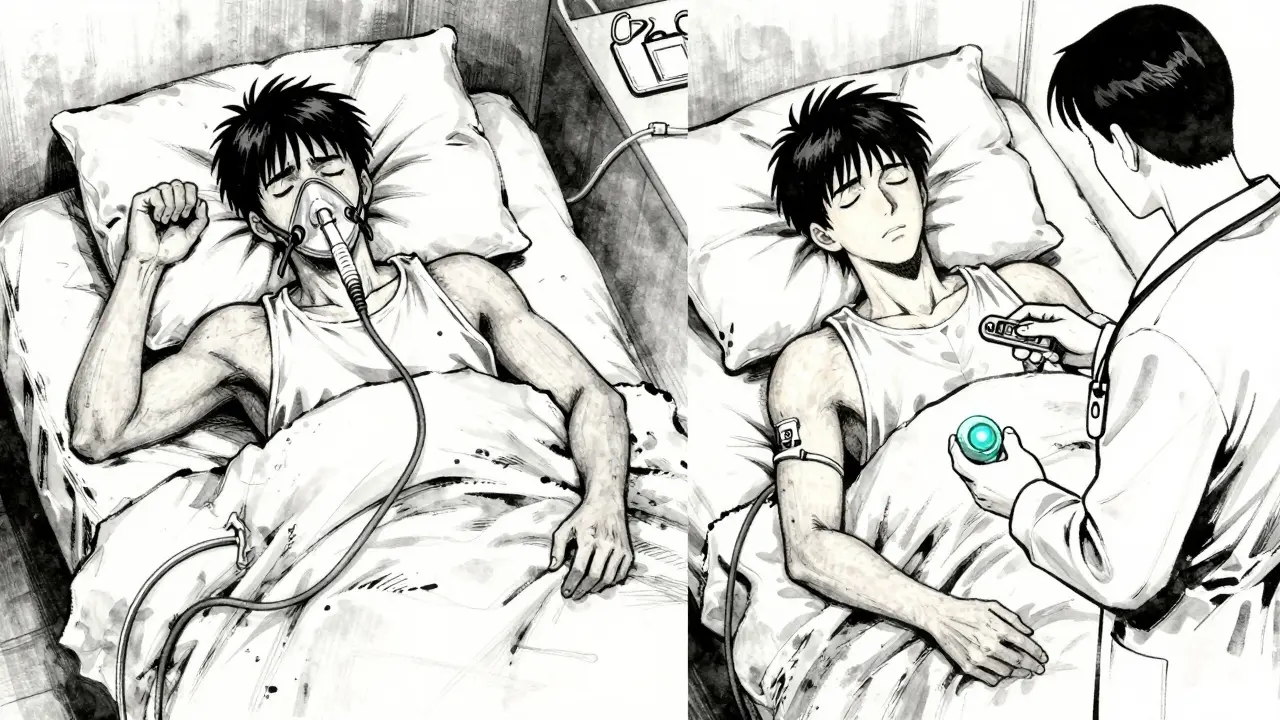
Think of Inspire as a pacemaker for your tongue. The device doesn’t push air into your throat like CPAP. Instead, it senses when you’re breathing in and sends a gentle pulse to the nerve that controls your tongue. This moves your tongue forward just enough to stop it from blocking your airway. No masks. No noise. No hoses. Just a small device working inside you while you sleep.
The system has three parts: a small generator implanted under your chest, a sensing wire that monitors your breathing, and a stimulation wire connected to the nerve behind your tongue. All of it is placed during a single outpatient surgery. After about a month of healing, your doctor turns it on. You use a remote control to turn it on before bed and off when you wake up. It’s that simple.
Who Is It For? The Right Candidates
This isn’t a first-line treatment. You have to have tried CPAP and failed. But beyond that, there are strict criteria. You need to be between 22 and 65 years old, have moderate to severe obstructive sleep apnea (AHI between 15 and 100), and have a body mass index (BMI) under 35. Your airway must also have a specific type of blockage-mostly from your tongue collapsing backward, not from your soft palate completely closing.
Doctors use a special test called drug-induced sleep endoscopy to check this. It’s like a mini-sleep study where you’re lightly sedated and they look inside your throat to see exactly where the collapse happens. If your airway collapse is mostly at the back of your tongue, you’re likely a good candidate. If it’s mostly from your soft palate or you have a lot of central apneas (where your brain doesn’t signal you to breathe), this isn’t the right option.
How Effective Is It?
The data speaks for itself. In the main clinical trial, patients went from an average of 29 breathing pauses per hour down to just 9. That’s a 68% drop. Two out of three people saw their apnea cut in half or more. And these aren’t short-term results. Five years later, most patients still have the same level of improvement.
Daytime symptoms get better too. People report feeling less tired, more alert, and more focused. Bed partners notice the biggest change: snoring drops by 85%. One woman in Manchester told her doctor, “I haven’t heard my husband snore in three years. I actually sleep through the night now.”
Compared to CPAP, adherence is much higher. Most people use Inspire every night. CPAP users average less than 4 hours a night. With Inspire, you’re not fighting the device-you’re just turning it on like a light switch.
What About Surgery and Risks?
The surgery takes 2 to 3 hours and is done under general anesthesia. You’ll have three small incisions: one under your jaw for the nerve, one lower on your neck for the breathing sensor, and one below your collarbone for the battery. Most people go home the same day. Recovery is quick-most are back to work in a week.
Complications are rare. Less than 0.5% of patients have a serious issue like infection or nerve damage. About 5% feel temporary tongue weakness, but it fades within weeks. Minor swelling or soreness at the incision sites is normal and goes away on its own.
The device is reversible. If you decide you don’t like it, the generator and wires can be removed. Unlike jaw surgery or tonsil removal, your anatomy isn’t permanently changed. You’re not locked into this forever.
How It Compares to Other Treatments
| Treatment | Effectiveness (AHI Reduction) | Adherence Rate | Surgery Required? | Long-Term Use |
|---|---|---|---|---|
| CPAP | 70-90% | 54-71% | No | Yes, nightly |
| Oral Appliances | 40-60% | 60-70% | No | Yes, nightly |
| UPPP (Throat Surgery) | 40-50% | High | Yes | Permanent |
| Inspire UAS | 65-70% | 90% | Yes | Yes, nightly |
Unlike UPPP or other throat surgeries, Inspire doesn’t remove tissue. It doesn’t change your anatomy. It just helps your body work the way it should. And unlike oral appliances, which only help mild cases or those with jaw structure issues, Inspire works for moderate to severe cases regardless of jaw shape.
Cost and Insurance Coverage
The total cost of the procedure-device, surgery, hospital stay-is around $35,000 to $40,000. That sounds high, but it’s comparable to what most people spend on CPAP over 5 years: masks, tubing, filters, repairs, and replacement machines.
Insurance coverage has improved dramatically. Medicare covers it for eligible patients. Most private insurers do too-85% of commercially insured people now have access. Before 2020, only a handful of plans covered it. Now, it’s standard for those who meet the criteria.
Some patients worry about hidden costs, like follow-up visits or remote programming. But these are included in the package. Inspire’s patient support team even offers 24/7 help if you have questions about the remote or the device settings.

Real-Life Challenges
It’s not perfect. Some people forget to turn it on at night. Others feel a slight tingling or twitching at first. It takes a few weeks to get used to the sensation. One user on a UK patient forum said, “I kept turning it off because I thought it wasn’t working. Turns out, I just needed to wait-it’s subtle.”
You need to be responsible about the remote. Lose it, and you’ll need to order a replacement. But the device won’t turn on without it. There’s no auto-start feature. You have to remember to use it every night. For some, that’s a hurdle. For others, it’s a small price to pay for a full night’s sleep.
What’s Next for This Therapy?
In 2023, the FDA expanded eligibility to include patients with BMI up to 40 and AHI up to 100. That opened the door for thousands more people who were previously turned away.
Researchers are working on smaller devices, longer battery life, and even AI tools to predict who will respond best. One hospital in London is testing a system that uses AI to analyze your airway scan and give you a “success score” before you even consider surgery.
More doctors are learning how to implant it. Five years ago, only 50 centers in the U.S. offered it. Now, over 200,000 people worldwide have had the device implanted. The market is growing fast, and so is the confidence in it.
Is It Right for You?
If you’ve tried CPAP and quit because it felt like a prison, Inspire might be your way out. It’s not magic. It’s not for everyone. But for those who fit the profile-moderate to severe sleep apnea, failed CPAP, BMI under 35, and tongue-based blockage-it’s one of the most effective options available.
Start by talking to a sleep specialist. Ask for a sleep study if you haven’t had one in the last two years. Then ask for a referral to a center that does drug-induced sleep endoscopy. If your airway collapse matches the pattern, you’re likely a candidate.
Sleep apnea isn’t just about snoring. It’s linked to high blood pressure, heart disease, and stroke. If you’ve been ignoring it because CPAP didn’t work, don’t give up. There’s another option. And for many, it’s life-changing.
Is upper airway stimulation the same as a pacemaker?
It works similarly to a pacemaker-it’s an implanted device that sends electrical pulses to regulate a body function. But instead of controlling your heartbeat, it controls your tongue movement during sleep to keep your airway open. The technology is adapted from cardiac devices but designed specifically for sleep apnea.
Can I have an MRI after getting Inspire therapy?
Yes, but only under specific conditions. The Inspire device is MRI-conditional, meaning you can have an MRI scan, but only if the machine is set to certain settings and the device is turned off beforehand. Always inform your radiologist that you have an implanted sleep device before any scan.
Does Inspire therapy cure sleep apnea?
No, it doesn’t cure it. It manages it. Like taking blood pressure medication, you need to keep using it to keep the benefits. If you stop using the device, your apnea will return. But for most people, the reduction in breathing pauses is so significant that it feels like a cure.
How long does the battery last?
The generator’s battery lasts about 11 years on average. When it runs low, your doctor replaces just the generator in a simple outpatient procedure. The leads (wires) stay in place. You won’t need another major surgery.
Can I travel with the device?
Yes. The remote control is small and easy to carry. Airport security scanners won’t trigger alarms, but you may be asked to show your patient ID card. The device doesn’t interfere with cell phones, Wi-Fi, or other electronics. You can use it anywhere.
What if I gain weight after the implant?
Weight gain can reduce the effectiveness of the device. The therapy works best when your BMI is under 35. If you gain weight, your airway may narrow again, and you might need to adjust the stimulation level or consider other treatments. Maintaining a healthy weight helps the device work better long-term.
If you’re tired of struggling with sleep apnea and CPAP isn’t working, Inspire therapy offers real hope. It’s not a quick fix, but for the right person, it’s the most reliable path back to restful sleep.


Mussin Machhour
December 24, 2025 AT 17:38This thing is a game-changer. I tried CPAP for six months and hated every second-felt like I was sleeping with a vacuum cleaner on my face. Then I got Inspire. No mask, no noise, just me and my pillow. I’ve slept through the night for two years straight. My wife says I stopped snoring like a chainsaw. Best decision I ever made.
Carlos Narvaez
December 26, 2025 AT 00:52It’s not magic. It’s just a fancy neuromodulator with a marketing budget. CPAP works if you actually use it. Most people just lack discipline.
Winni Victor
December 26, 2025 AT 06:17Oh wow, another corporate-funded miracle cure. Next they’ll sell us a brain chip that makes us love our jobs. This isn’t therapy-it’s a $40k luxury upgrade for people who can’t handle a little discomfort. And don’t get me started on the battery. Eleven years? Yeah right. That’s when they’ll start charging you $200 a month for ‘cloud sync’.
Terry Free
December 26, 2025 AT 06:36Let’s be real. If you’re obese and still think this is a fix, you’re deluding yourself. This doesn’t solve the root problem-it just masks it with electrodes. And yes, I’m one of those people who actually used CPAP for 7 hours a night. You don’t get to opt out of responsibility because the mask is ‘uncomfortable’.
Lindsay Hensel
December 27, 2025 AT 21:45As someone who has witnessed a close family member undergo this procedure, I can say with absolute certainty that the transformation in quality of life is profound. The dignity restored-sleeping beside a loved one without fear of waking them-is priceless. This is medicine at its most humane.
Linda B.
December 29, 2025 AT 04:09Did you know the FDA approved this because Medtronic donated to a senator’s campaign? The real reason they pushed this is so insurance companies can stop paying for CPAP machines. They’re replacing one product with a more expensive one. And don’t even get me started on the MRI restrictions-what if you need a scan and your device is dead? You’re screwed. They don’t tell you that part
Oluwatosin Ayodele
December 30, 2025 AT 13:49In Nigeria we don’t even have CPAP machines in most hospitals. You’re talking about a $40,000 implant like it’s a phone upgrade. This isn’t medicine-it’s a privilege for the rich. Meanwhile, people here die because they can’t afford a simple mask. Your ‘life-changing’ solution is a joke to the rest of the world.
Jason Jasper
December 30, 2025 AT 20:12I’ve had it for 18 months. The tingling took a while to get used to, but now I don’t even notice it. I used to wake up gasping. Now I wake up feeling rested. It’s not perfect, but it’s the first thing in years that actually worked. I’m not a fan of surgery, but this was worth it.
Bailey Adkison
December 31, 2025 AT 00:29Contrary to popular belief, Inspire does not cure sleep apnea. It manages it. You must use it nightly. Failure to do so results in recurrence. The device is not a substitute for lifestyle change. Weight gain diminishes efficacy. This is not a cure. It is a tool. Use it correctly or don’t bother.
Ben Harris
January 1, 2026 AT 18:11Okay but have you seen the TikTok influencers who say this is ‘the new glow up’? I swear I saw one guy post a video with his remote like it was an iPhone and say ‘I’m not sleeping without my Inspire baby’-like it’s a designer accessory. This is not a lifestyle brand. It’s a medical implant. People are turning a life-saving device into a flex. I’m not mad, I’m just disappointed
Harbans Singh
January 2, 2026 AT 03:01I’m from India and I’ve seen people here struggle with CPAP for years because they can’t afford replacements or clean filters. I’m curious-does Inspire work the same way for people with different facial structures? In South Asia, airway anatomy is often different. Has there been any research on this outside the US and Europe? I’d love to see data from diverse populations. This could help so many if it’s truly adaptable.