When it comes to losing weight with medication, the landscape has changed dramatically in the last few years. What used to be a limited selection of pills with modest results is now dominated by powerful injectables that can help people lose up to 20% of their body weight. But just because a new drug works better doesn’t mean it’s right for everyone. The real question isn’t whether GLP-1 agonists are more effective-it’s whether they’re the right choice for your life, budget, and health goals.
How GLP-1 Agonists Actually Work
GLP-1 agonists like Wegovy, Zepbound, and Saxenda don’t just suppress your appetite. They mimic a natural hormone your body already makes after eating-glucagon-like peptide-1. This hormone tells your brain you’re full, slows down how fast your stomach empties, and helps your pancreas release insulin only when needed. The result? You eat less, feel satisfied longer, and your blood sugar stays steadier.
These drugs weren’t designed for weight loss at first. They were created for type 2 diabetes. But doctors noticed something surprising: patients lost a lot of weight. That led to FDA approval for weight management in 2021 with Wegovy, followed by Zepbound in 2023. Today, they’re the most prescribed weight loss medications in the U.S., making up nearly 80% of new prescriptions.
Older Weight Loss Drugs: What’s Still Out There
Before GLP-1 agonists, the options were limited and often underwhelming. Orlistat (Alli, Xenical) blocks fat absorption in your gut-so about 30% of the fat you eat passes through undigested. That means greasy stools, frequent bathroom trips, and the need to take it with every meal. It typically leads to 5-10% weight loss, but only if you stick to a low-fat diet.
Phentermine-topiramate (Qsymia) combines a stimulant with an anti-seizure drug to reduce hunger and boost metabolism. It can help people lose around 10% of their body weight, but side effects include dry mouth, tingling in hands and feet, and increased heart rate. Naltrexone-bupropion (Contrave) targets brain reward pathways to reduce cravings. It’s taken daily as a pill and usually results in 5-8% weight loss.
Phentermine alone is still prescribed, often for short-term use. It’s cheap-sometimes under $50 a month-but carries risks like high blood pressure and insomnia. None of these older drugs offer the same level of weight loss as GLP-1 agonists, and many come with more annoying side effects.
Weight Loss Results: The Numbers Don’t Lie
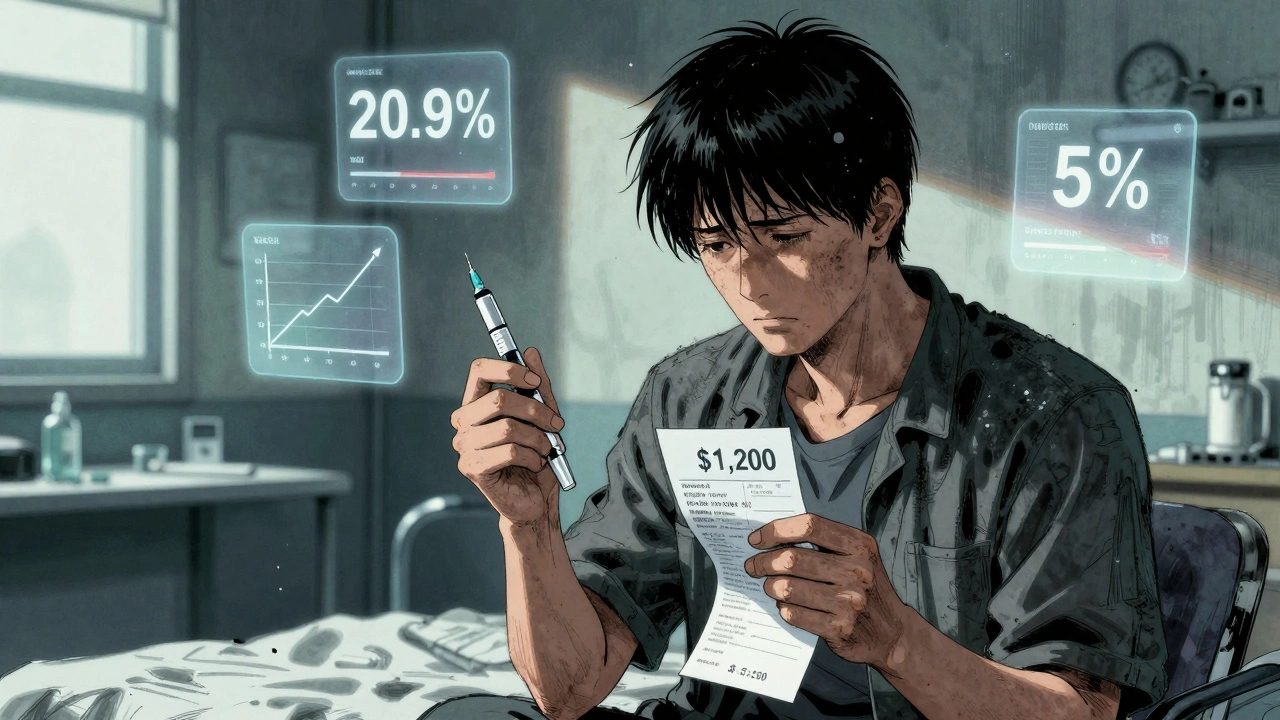
Let’s compare real outcomes. In clinical trials, Wegovy (semaglutide) led to an average weight loss of 14.7% after 68 weeks. Zepbound (tirzepatide) hit 20.9% over 72 weeks. That’s not just losing a few pounds-it’s dropping from a size 14 to a size 8 for many people.
Compare that to Saxenda (liraglutide), an earlier GLP-1 drug: 8% weight loss. Orlistat: 5-10%. Qsymia: about 10%. Contrave: 5-8%. Even the best of the older drugs fall short.
But here’s the catch: real-world results are lower than trial numbers. A 2024 study from NYU Langone found people on GLP-1 medications lost just 4.7% after six months and 7% after one year. Why? Many stop taking them. Side effects, cost, or just not seeing fast enough results lead to high dropout rates-up to 70% within a year.

Cost and Insurance: The Hidden Barrier
GLP-1 agonists cost $1,000 to $1,400 a month without insurance. Even with manufacturer coupons, you might still pay $500-$900 a month. Most insurance plans won’t cover them for weight loss unless you have diabetes or a BMI over 40 (or 35 with other health problems like high blood pressure or sleep apnea).
Older drugs? Much cheaper. Phentermine can cost as little as $10-$30 a month. Orlistat is $50-$150. Qsymia and Contrave are more expensive-around $150-$300-but still far below GLP-1s. And many insurers cover them without strict restrictions.
That price gap is why so many people can’t stay on GLP-1s long-term. A 2024 KFF survey found 62% of users struggled to afford them. Some turn to online pharmacies or import versions from other countries-risky moves that can lead to fake or unsafe products.
Side Effects: What You’ll Actually Feel
GLP-1 agonists aren’t magic. Nausea affects 20-50% of users, especially when starting or increasing the dose. Vomiting, diarrhea, constipation, and stomach pain are common. Some people report severe gastroparesis-delayed stomach emptying-that lasts for weeks. That’s why doctors start patients on low doses and slowly increase over 4-5 months.
Older drugs have their own issues. Orlistat causes oily spotting and urgent bowel movements. Phentermine can raise your heart rate and cause anxiety. Qsymia has been linked to birth defects and requires monthly pregnancy tests for women of childbearing age. Contrave can increase the risk of seizures in people with a history of them.
For many, the side effects of GLP-1s are manageable with time. But for others, they’re unbearable. Reddit communities like r/Wegovy and r/Ozempic are full of people sharing their experiences-some praising the results, others saying they quit because they couldn’t eat without feeling sick.

Who Benefits Most from GLP-1 Agonists?
GLP-1s are best for people who:
- Have a BMI of 30 or higher (or 27 with weight-related health issues)
- Want to lose 15% or more of their body weight
- Can handle weekly injections
- Have insurance coverage or can afford the cost
- Are willing to make lifestyle changes (meds don’t work alone)
They’re especially helpful for people with type 2 diabetes, since they improve blood sugar control too. They’re also a good option for those who want to avoid surgery but need more than what older pills can offer.
But they’re not ideal for people who:
- Can’t tolerate nausea or digestive issues
- Have a history of medullary thyroid cancer or multiple endocrine neoplasia
- Are pregnant or planning to become pregnant
- Can’t afford the cost or are denied insurance coverage
- Expect quick results without changing their diet or activity level
What Comes Next? The Future of Weight Loss Drugs
Science isn’t standing still. Retatrutide, a triple agonist targeting GLP-1, GIP, and glucagon, showed 24.2% weight loss in early trials. MariTide, a new antibody-based drug, is now in Phase 3 testing and could hit the market by 2027.
But even these next-gen drugs won’t solve the biggest problems: cost and access. Experts warn that without major changes in insurance coverage and pricing, these drugs will remain out of reach for most Americans. Some predict that by 2027, GLP-1s will control 85% of the prescription weight loss market-but only for those who can pay.
Meanwhile, bariatric surgery still wins for long-term results. A 2024 study found surgery patients lost 24% of their body weight after two years-nearly triple what most GLP-1 users achieve in the same time. And surgery’s effects tend to last longer, even after stopping meds.
What Should You Do?
If you’re considering weight loss medication, start with your doctor. Don’t just ask for Wegovy or Zepbound. Ask: What’s my goal? Can I afford this? What side effects am I willing to live with? Am I ready to make lasting changes?
GLP-1 agonists are powerful tools-but they’re not a shortcut. They work best when paired with better eating habits, regular movement, and mental health support. If you can’t stick with them, the weight will come back. Studies show 50-100% of people regain lost weight after stopping these drugs.
Older medications aren’t glamorous, but they’re affordable, proven, and work for some people. There’s no single best drug. The best one is the one you can take consistently, affordably, and safely.
Are GLP-1 agonists better than older weight loss drugs?
Yes, in terms of weight loss effectiveness. GLP-1 agonists like Wegovy and Zepbound typically lead to 15-20% body weight loss in clinical trials, while older drugs like orlistat, Qsymia, and Contrave usually result in 5-10%. GLP-1s also improve blood sugar and reduce cardiovascular risk. But they’re more expensive, require injections, and cause more gastrointestinal side effects.
Can I take GLP-1 agonists without insurance?
It’s possible, but very expensive. Without insurance, monthly costs range from $1,000 to $1,400. Some manufacturers offer savings cards that cap your annual out-of-pocket cost at $500-$1,000, but these don’t cover the full price. Many people turn to international pharmacies or patient assistance programs, but those carry risks or strict eligibility rules.
Do GLP-1 agonists work for everyone?
No. About 20-50% of users experience nausea, vomiting, or diarrhea, especially when starting or increasing the dose. Around 70% of people stop taking them within a year due to side effects, cost, or lack of results. They’re also not recommended for people with certain thyroid cancers or a personal or family history of medullary thyroid cancer.
How long do I need to take GLP-1 agonists?
They’re meant for long-term use. Stopping the medication almost always leads to weight regain-studies show 50-100% of lost weight returns within a year. If you stop because of side effects or cost, you may regain all the weight you lost. Think of them like blood pressure or diabetes meds: they manage the condition but don’t cure it.
Can I switch from an older drug to a GLP-1 agonist?
Yes, but it should be done under medical supervision. Your doctor will likely stop your old medication first and start you on a low dose of the GLP-1 agonist, then gradually increase it over several months to reduce side effects. Never switch on your own-some combinations can be unsafe.
What if GLP-1 agonists don’t work for me?
You’re not alone. Many people don’t lose enough weight or can’t tolerate the side effects. In those cases, older medications, lifestyle changes, or bariatric surgery may be better options. Surgery still offers the most durable results for severe obesity. Talk to your doctor about all available paths-not just the newest drug.

Karandeep Singh
December 2, 2025 AT 11:59glp-1s are just fancy appetite suppressants with a $1k price tag
Debbie Naquin
December 2, 2025 AT 12:07The neuroendocrine modulation of satiety signaling via GLP-1 receptor agonism represents a paradigm shift in metabolic pharmacotherapy-but the economic externalities and access inequities render this innovation functionally exclusionary for the majority of the population. The pharmacodynamic superiority is undeniable, yet the sociopolitical architecture of healthcare commodification negates its therapeutic potential.
elizabeth muzichuk
December 4, 2025 AT 12:01People act like these drugs are a miracle when really they’re just a Band-Aid on a broken system. You think you’re winning when you lose 20% but you’re just trading one addiction for another-now you’re addicted to a $1200 monthly injection instead of cookies. And don’t get me started on how the pharma companies are laughing all the way to the bank while people scramble for counterfeit vials off Telegram. This isn’t medicine, it’s capitalism with a syringe.
Charlotte Collins
December 5, 2025 AT 02:02Let’s be real-the real story isn’t the drugs, it’s the fact that we’ve turned weight loss into a pharmaceutical arms race instead of fixing food deserts, mental health access, and the cultural obsession with thinness. People aren’t failing because they can’t afford Wegovy-they’re failing because the system never gave them a chance to begin with. And now we’re selling hope in vials while ignoring the root causes.
Erin Nemo
December 5, 2025 AT 20:19My cousin lost 30 lbs on semaglutide but quit after 4 months because she couldn’t eat dinner without feeling like she was going to throw up. Now she’s back to where she started. It’s not magic. It’s just… hard.
Scotia Corley
December 6, 2025 AT 23:06It is an objective fact that GLP-1 agonists have demonstrated superior efficacy in clinical trials. To suggest otherwise is to misunderstand the data. The issue is not the medication-it is the lack of patient adherence and the absence of comprehensive behavioral support structures. Without these, even the most effective pharmacotherapy will fail.
Mary Ngo
December 7, 2025 AT 15:10Did you know that the original GLP-1 research was funded by a pharmaceutical consortium with ties to a private equity firm that also owns a chain of weight-loss clinics? Coincidence? Or is this just another case of manufactured demand? The FDA approval process is a revolving door, and the data you see? It’s curated. The long-term cardiac outcomes? Still unpublished. The thyroid cancer risk? Buried in the fine print. Wake up.
Rachel Stanton
December 8, 2025 AT 05:18For those considering GLP-1s: don’t just focus on the number on the scale. Think about how you feel during the day-do you have energy? Are you sleeping better? Is your blood pressure improving? These drugs aren’t just for weight-they’re metabolic reset tools. But they’re not a solo act. Pair them with therapy, movement, and real nutrition. And if you can’t afford them? Talk to your provider about older meds. They’re not sexy, but they’re still valid tools. You’re not failing if you start small.
ariel nicholas
December 9, 2025 AT 17:25Why is it that every time a new drug comes out, Americans act like it’s the end-all-be-all? We’re a nation that can’t even afford insulin-and now we’re expected to pay $1,400 a month for a drug that makes you nauseous? Meanwhile, in Canada, they’ve got a public drug plan that covers this. But no, we’d rather let people go bankrupt than fix the system. This isn’t progress-it’s exploitation dressed up as innovation.
Margaret Stearns
December 11, 2025 AT 05:44i’ve been on orlistat for 6 months and lost 12 lbs. yeah it’s messy but i can afford it and my knees feel better. maybe the ‘better’ drug isn’t the one with the highest % loss but the one you can actually stick with.
amit kuamr
December 12, 2025 AT 02:56GLP-1s are overhyped. The real issue is insulin resistance and processed food. No pill fixes that. You need to change your diet. Period. These drugs just mask the problem until you stop taking them and then you gain back everything plus more. People need to stop looking for shortcuts and start eating real food.
James Allen
December 14, 2025 AT 02:42Look, I get it. The drugs work. But let’s not pretend this isn’t a privilege play. My buddy in Texas lost 50 lbs on Zepbound and now he’s got a whole Instagram page about it. Meanwhile, my sister in rural Alabama can’t even get a doctor to prescribe her phentermine. This isn’t healthcare-it’s a luxury good with a medical label. And don’t tell me it’s about health. If it was, we’d be fixing food deserts before we sell $1,000 shots.