When dealing with adverse drug events, any unwanted reaction that follows the use of a medication. Also known as ADEs, they range from mild nausea to severe organ injury. Knowing the details in drug labeling, the official information package that lists indications, dosing, and warnings and having a strong pharmacovigilance, the systematic process of detecting, assessing, and preventing drug‑related problems framework are essential for protecting patient safety, the overall well‑being of individuals who receive medical treatment.
Regulators in the US and Europe often write different warnings for the same drug. For example, the EMA may require a specific heart‑failure note that the FDA does not, creating a labeling gap that can lead to unexpected adverse drug events. Those gaps matter because clinicians rely on the label to spot potential interactions, like the well‑documented risk of bleeding when Coumadin is combined with certain antibiotics. When a label omits such information, patients can experience serious complications that could have been avoided. This is why pharmacovigilance teams monitor post‑marketing reports and feed new findings back into updated labeling.
Beyond official documents, everyday clinical practice adds layers of insight. A nurse who notices that azithromycin often triggers stomach upset may report that symptom, prompting a label tweak that warns future users. Similarly, patients on disulfiram for alcohol dependence benefit from strong social support; without it, the drug’s intended effect can be undermined, leading to relapse and potential toxicity. Real‑world observations—whether from a sleep study linking REM disruption to chronic pain medication use or from a hospital’s cost analysis of organ‑rejection therapies—feed the safety loop and reduce the chance of ADEs.
Technology also plays a role. Electronic health records flag interactions between drugs like doxycycline and warfarin, while mobile apps let patients log side‑effects in real time. These tools translate raw data into actionable alerts, helping clinicians adjust therapy before an adverse event escalates. In short, the ecosystem of drug labeling, pharmacovigilance reporting, and digital monitoring works together to keep patients safe.
When you browse the collection below, you’ll see how each article illustrates a piece of this safety puzzle. From deep dives into labeling differences between the EMA and FDA, to cost‑impact studies of organ‑rejection treatments, to practical guides on buying cheap generic medications safely, the posts highlight the many ways adverse drug events can be identified, reported, and prevented. Whether you’re a health‑care professional, a patient managing multiple prescriptions, or just curious about how medicines are kept in check, the insights here will give you a clearer picture of the risks and the safeguards built around them.
Ready to see the details? Below you’ll find a curated list of articles that unpack specific ADE scenarios, compare drug safety profiles, and offer tips for staying ahead of potential problems. Dive in and discover how better labeling, vigilant monitoring, and informed choices work together to minimize adverse drug events.
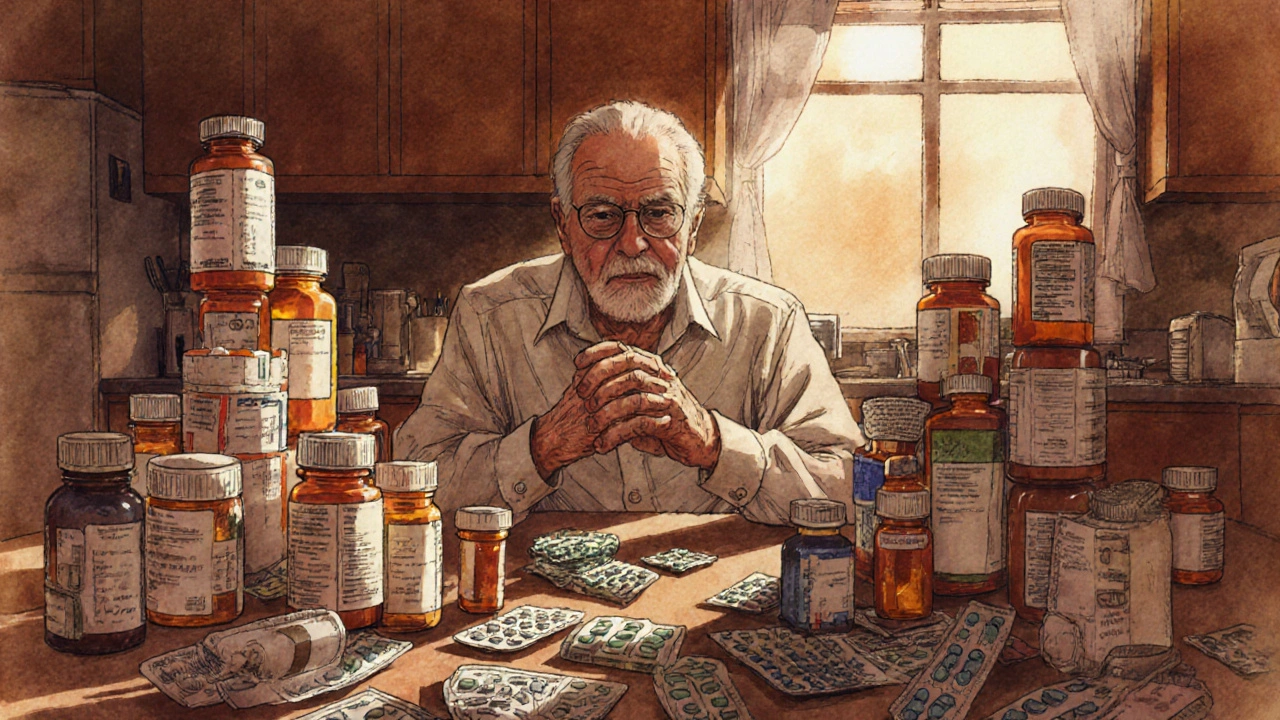
Learn how to identify, assess, and safely reduce geriatric polypharmacy with proven medication reviews, deprescribing tools, and cost‑saving strategies.
Read More >>