When working with deprescribing, the systematic process of tapering, stopping, or substituting medicines that cause more harm than benefit. Also known as medication withdrawal, it helps patients avoid side effects and drug interactions.
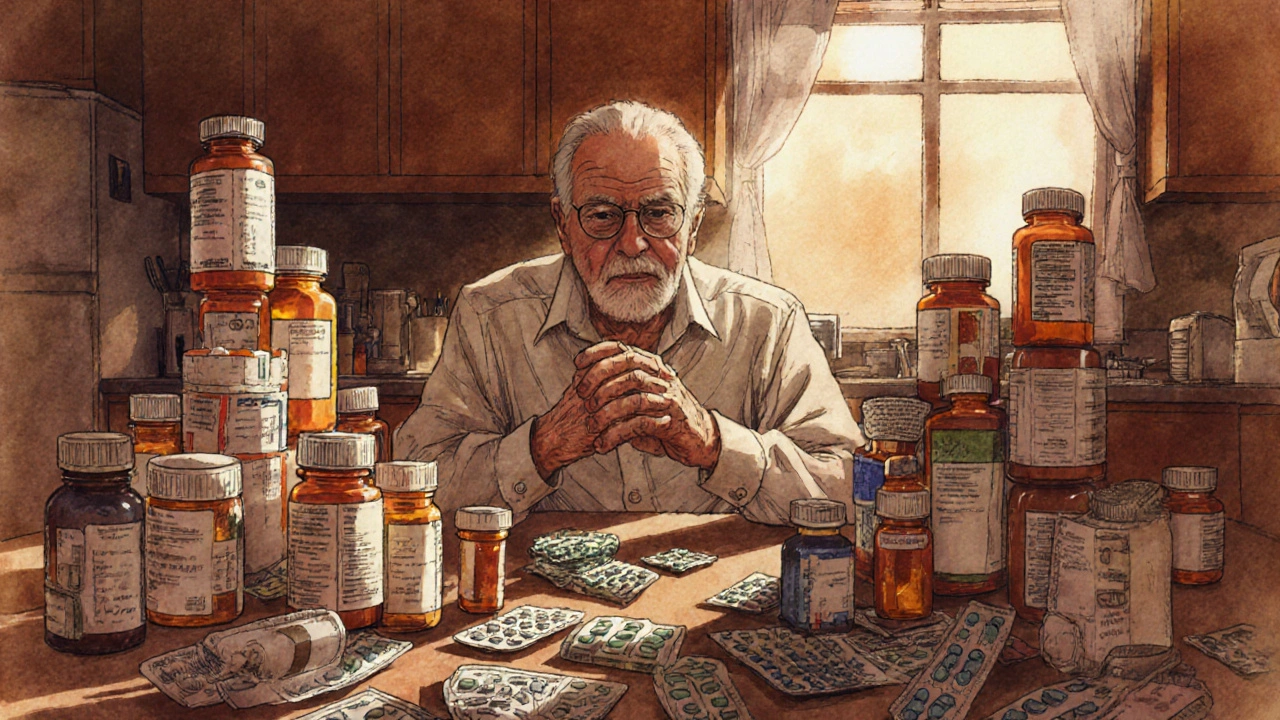
One of the biggest drivers behind deprescribing is polypharmacy, the use of multiple concurrent drugs, often leading to adverse events, drug‑drug interactions, and higher healthcare costs. Clinicians tackle polypharmacy by conducting a thorough medication review, a structured assessment that checks each prescription for current need, appropriate dosage, and safety profile. This review acts as the first checkpoint in any deprescribing effort, ensuring that decisions are based on solid evidence rather than habit.
National clinical guidelines, official recommendations that synthesize research, expert opinion, and patient values provide the roadmap for safe deprescribing. Guidelines from bodies like the American Geriatrics Society or NICE outline criteria for stopping specific drug classes, suggest tapering schedules, and highlight situations where a medication should never be discontinued. By aligning practice with these guidelines, clinicians reduce the risk of withdrawal syndromes and maintain therapeutic goals.
Patient safety sits at the heart of every deprescribing decision. When a drug is reduced or stopped, clinicians monitor for rebound symptoms, withdrawal effects, or disease flare‑ups. Tools such as the STOPP/START criteria or the Beers List help identify high‑risk medications in older adults. Combining these tools with a shared decision‑making conversation puts the patient’s preferences front and center, building trust and improving adherence to the new regimen.
Implementing a deprescribing plan often follows a step‑wise protocol: 1) Identify the target medication, 2) Evaluate the indication and risk‑benefit ratio, 3) Choose an appropriate tapering strategy, and 4) Set up follow‑up appointments to assess response. For drugs with short half‑lives, a simple stop may suffice, whereas long‑acting agents like benzodiazepines or opioids require a gradual reduction to avoid withdrawal.
Successful deprescribing rarely happens in isolation. Pharmacists, nurses, and primary‑care physicians form an interdisciplinary team that shares observations, adjusts doses, and educates the patient. This collaborative approach ensures that each professional’s expertise feeds into a cohesive plan, making the process smoother and more reliable.
Monitoring outcomes is the final piece of the puzzle. Clinicians track metrics such as reduced adverse drug events, improved quality‑of‑life scores, or lowered healthcare utilization. These data not only validate the deprescribing effort but also inform future guidelines and institutional policies.
The articles below dive deeper into each of these areas—showing how drug labeling differences affect prescribing, the economic impact of organ rejection treatments, and practical comparisons of common medications—all of which provide valuable context for anyone looking to refine their deprescribing practice.
Learn how to identify, assess, and safely reduce geriatric polypharmacy with proven medication reviews, deprescribing tools, and cost‑saving strategies.
Read More >>