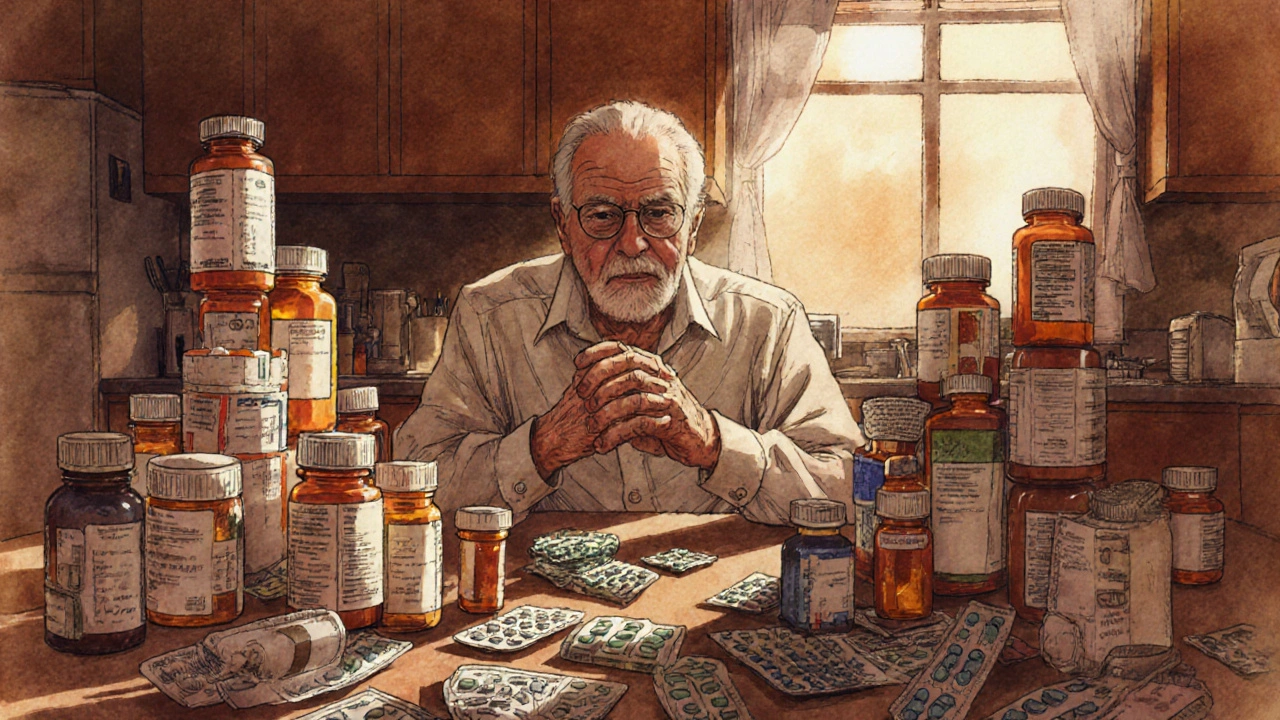
When dealing with geriatric polypharmacy, the concurrent use of five or more prescription or OTC drugs by older adults. Also known as multiple drug therapy in seniors, it creates a complex medication landscape that can overwhelm patients and clinicians alike. A major challenge is medication adherence, the ability of patients to take each drug as prescribed. When dozens of pills are scheduled throughout the day, missing doses or taking them at the wrong time becomes common. Equally concerning are drug interactions, the chemical or physiological effects that occur when two or more medications influence each other. These interactions can amplify side‑effects, reduce therapeutic benefits, or trigger dangerous events such as bleeding or heart rhythm problems. To cut through the confusion, many clinicians turn to deprescribing, a systematic process of reviewing and safely stopping medications that are no longer needed. By combining clear definitions with real‑world tools, patients and providers can start to untangle the medication web that defines geriatric polypharmacy.
Every additional drug raises the chance of an adverse drug event, a term that covers anything from mild nausea to life‑threatening organ damage. Studies show that seniors on ten or more medications are twice as likely to be hospitalized for drug‑related problems compared with those on fewer drugs. The risk isn’t just about numbers; it’s about the types of drugs, their dosing schedules, and the underlying health conditions they aim to treat. For example, a blood thinner combined with a non‑steroidal anti‑inflammatory can double bleeding risk, while certain antidepressants may interfere with heart‑rate‑controlling beta‑blockers. Clinical guidelines such as the Beers Criteria and the STOPP/START tools were created precisely to flag high‑risk combos in older patients. Health systems are also investing in electronic medication reconciliation systems that alert prescribers at the point of care, helping to catch dangerous overlaps before they reach the patient. The bottom line: geriatric polypharmacy is a major driver of preventable harm, and understanding its ripple effects is the first step toward safer care.
So, how do you move from a tangled pill box to a streamlined regimen? Start with a comprehensive medication review — ideally led by a pharmacist or geriatrician — that inventories every prescription, supplement, and over‑the‑counter product. Next, apply deprescribing principles: identify drugs with limited benefit, prioritize those with the highest interaction potential, and taper or stop them under close monitoring. Incorporate patient‑centered goals; ask seniors what outcomes matter most to them, whether it’s mobility, cognition, or simply fewer side‑effects. Finally, use supportive tools like medication calendars, pill organizers, and mobile reminders to boost adherence once the list is trimmed. Below, you’ll find articles that dive deep into specific drug comparisons, regulatory nuances, and practical tips that together form a toolbox for tackling geriatric polypharmacy head‑on.
Learn how to identify, assess, and safely reduce geriatric polypharmacy with proven medication reviews, deprescribing tools, and cost‑saving strategies.
Read More >>